What Are the 10 Types of Mental Disorders?
-
 By:
Valerie Puffenberger, PMHNP-BC
By:
Valerie Puffenberger, PMHNP-BC
-
 Editor:
Phyllis Rodriguez, PMHNP-BC
Editor:
Phyllis Rodriguez, PMHNP-BC
-
 Clinical Reviewer:
Dr. Ash Bhatt, MD, MRO
Clinical Reviewer:
Dr. Ash Bhatt, MD, MRO
Mental health affects every aspect of everyday life—from how we think and feel to how we handle stress, relate to others, and make decisions. Yet despite how common mental health issues are, confusion about what qualifies as a mental disorder remains widespread.
This guide breaks down the 10 types of mental disorders most frequently discussed in clinical practice and public health. You’ll learn what distinguishes each category, who they affect, and what singular and dual diagnosis treatment options exist. Whether you’re researching for yourself, supporting a loved one, or simply expanding your knowledge, understanding these conditions is the first step toward reducing stigma and promoting recovery.
Key Takeaways
- Mental disorder is an umbrella term covering hundreds of diagnoses, but they can be organized into 10 major categories that account for most commonly discussed mental health conditions.
- The 10 types include anxiety disorders, depressive disorders, bipolar and related disorders, schizophrenia spectrum and other psychotic disorders, trauma- and stressor-related disorders, obsessive-compulsive and related disorders, eating disorders, personality disorders, neurodevelopmental disorders, and substance-related and addictive disorders.
- Millions of people worldwide live with these conditions—roughly 1 in 8 people globally were living with a mental disorder in 2019, according to the World Health Organization.
- Recovery and effective treatment are possible for most mental health conditions, and seeking help is a sign of strength rather than weakness.
- If you or someone you know is experiencing suicidal thoughts or is in immediate crisis, please contact local emergency services or a crisis hotline right away.
What Are Mental Disorders? (Quick Overview)
Mental disorders are clinically significant disturbances in thinking, emotion regulation, or behavior that cause distress or significant impairment in work, school, or personal relationships. This definition comes from modern diagnostic manuals like the DSM-5-TR (Diagnostic and Statistical Manual of Mental Disorders) and ICD-11 (International Classification of Diseases).
Here’s what you need to know upfront:
| Fact | Detail |
|---|---|
| Total diagnoses | Over 200 specific mental health conditions exist in official classification systems |
| Global prevalence | In 2019, about 1 in 8 people worldwide (roughly 970 million) lived with a mental disorder |
| U.S. statistics | Approximately 1 in 5 American adults experience a mental illness each year |
| Range of severity | Mental disorders span from mild and short-term to severe and lifelong |
| Who’s affected | People of all ages, genders, ethnicities, and socioeconomic backgrounds |
Diagnosis requires evaluation by qualified mental health professionals through thorough medical and psychological assessment. Online reading can increase awareness, but it cannot replace professional diagnosis.
The 10 categories covered in this article organize the landscape of mental health disorders into manageable groups, helping you understand how different conditions relate to one another.
1. Anxiety Disorders
Anxiety disorders are the most common mental disorders globally. They involve excessive fear, worry, or avoidance that interferes with daily life far beyond normal nervousness or stress.
Key Types of Anxiety Disorders
- Generalized anxiety disorder (GAD): Persistent excessive worry about various aspects of life, often accompanied by physical symptoms
- Panic disorder: Recurrent unexpected panic attacks with intense physical symptoms
- Social anxiety disorder: Intense fear of social situations and being judged by others
- Specific phobias: Irrational fear of particular objects or situations (heights, spiders, flying)
- Separation anxiety disorder: Excessive fear about separation from attachment figures
- Agoraphobia: Fear of situations where escape might be difficult
Common Symptoms
People with anxiety disorders often experience:
- Constant nervousness and restlessness
- Muscle tension and fatigue
- Panic attacks (racing heart, shortness of breath, sweating, trembling)
- Avoidance of feared situations
- Sleep disturbances
- Difficulty concentrating
- Feeling on edge or irritable
In 2021, an estimated 359 million people worldwide were living with an anxiety disorder, including tens of millions of children and adolescents.
Treatment Approaches
Effective treatments for anxiety include:
- Cognitive behavioral therapy (CBT)
- Exposure therapy
- Relaxation and mindfulness techniques
- Lifestyle changes (regular exercise, reduced caffeine, adequate sleep)
- Medications such as SSRIs or anti-anxiety drugs when appropriate
Left untreated, anxiety disorders can worsen and increase the risk of depression, substance use, and physical health problems.
2. Depressive Disorders
Depressive disorders go far beyond feeling sad after a difficult day. They represent persistent changes in mood, thinking, and physical functioning that significantly impair a person’s ability to live their life.
Main Types
- Major depressive disorder: Episodes of depressed mood lasting at least two weeks with significant functional impairment
- Persistent depressive disorder (dysthymia): Chronic low-grade depression lasting two years or more
Core Symptoms
| Symptom Category | Examples |
|---|---|
| Mood | Depressed mood most of the day, feeling sad, empty, or hopeless |
| Interest | Loss of interest or pleasure in activities once enjoyed |
| Physical | Changes in appetite, weight, and sleep patterns; fatigue |
| Cognitive | Poor concentration, difficulty making decisions |
| Self-perception | Feelings of worthlessness or excessive guilt |
| Severe | Thoughts of death or suicide, self harm behaviors |
About 280 million people worldwide were living with depression in 2019, making it a leading contributor to global disability. Depression affects work performance, educational achievement, and personal relationships when untreated.
Treatment Options
- Psychotherapy (CBT, interpersonal therapy)
- Antidepressant medications
- Lifestyle interventions (exercise, regular sleep schedules, social support)
- Emerging treatments like ketamine/esketamine under medical supervision for treatment-resistant cases
3. Bipolar and Related Disorders
Bipolar disorders involve dramatic mood swings between depressive episodes and periods of elevated mood called mania or hypomania. These shifts affect mood, energy, judgment, and behavior in ways that can disrupt relationships, careers, and safety.
Types of Bipolar Disorder
- Bipolar I disorder: At least one manic episode (may include depressive episodes)
- Bipolar II disorder: Hypomanic episodes plus major depressive episodes, but no full mania
- Cyclothymic disorder: Chronic fluctuating mood with subthreshold hypomanic and depressive symptoms
Manic Episode Symptoms
During manic episodes, a person may experience:
- Abnormally high energy and decreased need for sleep
- Racing thoughts and pressured speech
- Inflated self-esteem or grandiosity
- Increased goal-directed activity
- Risky behaviors (excessive spending, risky sexual behavior)
- Sometimes psychotic features (delusions, hallucinations)
An estimated 37 million people worldwide lived with bipolar disorder in 2021. Lifetime prevalence is roughly 1-2% of adults.
Treatment Directions
Treatment typically includes:
- Mood stabilizers (lithium, valproate, lamotrigine)
- Atypical antipsychotics for acute mania
- Strict sleep routines and lifestyle stability
- Psychoeducation for patient and family
- Ongoing therapy and family support
Bipolar disorder carries significant suicide risk, making consistent treatment and monitoring essential.
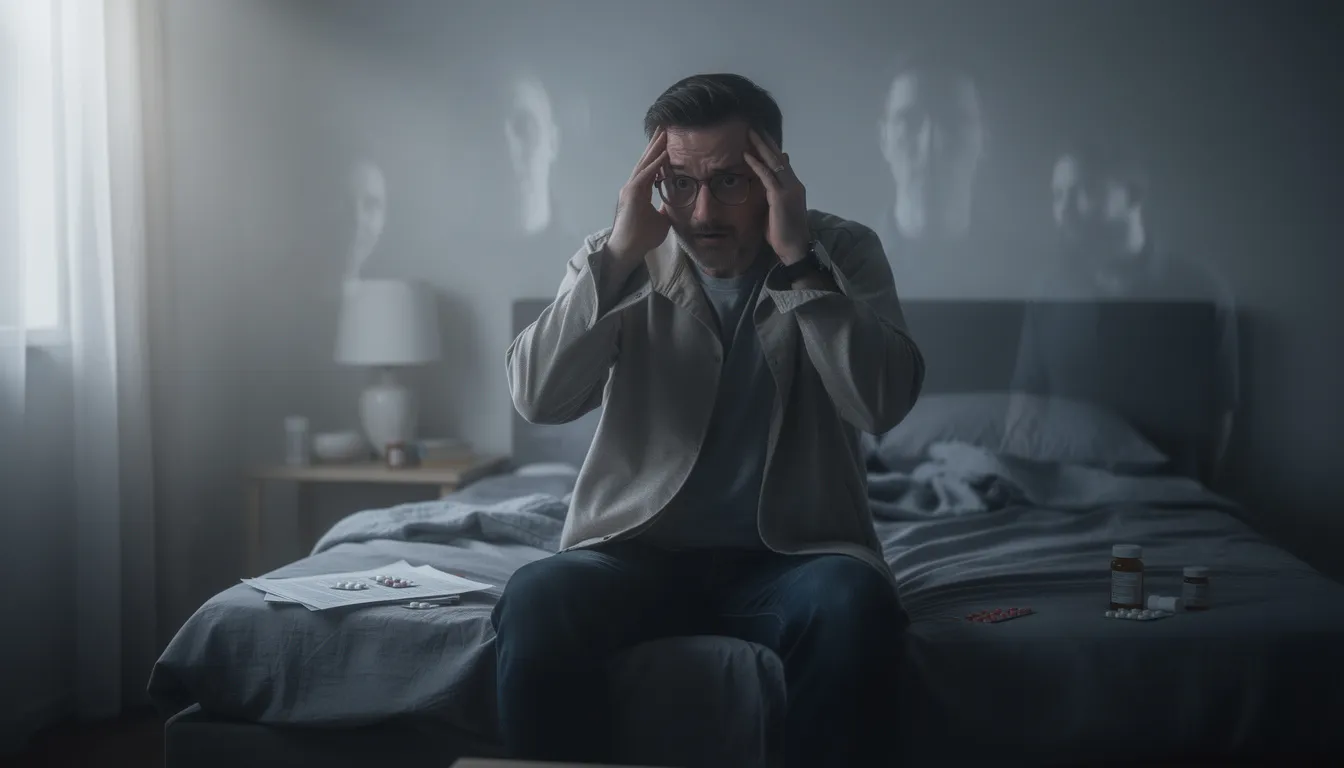
4. Schizophrenia Spectrum and Other Psychotic Disorders
Psychotic disorders significantly alter a person’s perception of reality. Schizophrenia is the best-known condition in this category, but the spectrum includes several related diagnoses.
Defining Features
| Symptom Type | Description |
|---|---|
| Positive symptoms | Hallucinations (often hearing voices), delusions (fixed false beliefs), disorganized speech |
| Negative symptoms | Lack of motivation, flat or blunted emotion, social withdrawal, reduced speech |
| Cognitive symptoms | Problems with attention, memory, and executive function |
Schizophrenia affects about 23-24 million people worldwide. Onset typically occurs in late adolescence or early adulthood (late teens to early 30s), with earlier onset more common in males.
Impact on Functioning
Psychotic disorders can severely impair:
- Self-care abilities
- Employment and education
- Relationships and social connections
- Physical health (life expectancy is reduced by 10-20 years on average)
Treatment Approaches
- Long-term antipsychotic medication
- Clozapine for treatment-resistant cases
- Psychoeducation for patients and families
- Supported housing and employment programs
- Early intervention services for first-episode psychosis
With appropriate treatment and support, many people with schizophrenia can manage symptoms and lead meaningful lives.
5. Trauma- and Stressor-Related Disorders (Including PTSD)
These disorders develop after exposure to highly stressful or traumatic events. Unlike normal stress reactions, symptoms persist long after the event and cause significant impairment.
Common Triggers
- Combat and war exposure
- Sexual assault or sexual abuse
- Serious accidents
- Natural disasters
- Chronic childhood abuse or neglect
- Witnessing violence
Post Traumatic Stress Disorder Symptoms
PTSD is the most widely recognized trauma-related condition. Core symptoms include:
- Intrusive symptoms: Flashbacks, nightmares, intrusive memories of the traumatic events
- Avoidance: Steering clear of reminders, people, or places associated with the trauma
- Negative changes: Persistent negative beliefs, emotional numbness, detachment from others
- Hyperarousal: Exaggerated startle response, hypervigilance, irritability, sleep problems
For PTSD diagnosis, symptoms must persist beyond one month and cause significant distress or impairment.
Research from the 2000s and 2010s documented particularly high PTSD rates among combat veterans, survivors of sexual violence, first responders, and populations affected by major natural disasters.
Evidence-Based Treatments
- Trauma-focused CBT
- EMDR (Eye Movement Desensitization and Reprocessing)
- Prolonged exposure therapy
- Medications for associated anxiety, depression, or sleep problems
6. Obsessive-Compulsive and Related Disorders
This group includes conditions where repetitive thoughts and behaviors dominate daily life and cause significant distress.
Conditions in This Category
- Obsessive compulsive disorder (OCD): Intrusive thoughts plus repetitive rituals
- Body dysmorphic disorder: Preoccupation with perceived flaws in appearance
- Hoarding disorder: Persistent difficulty discarding possessions
- Trichotillomania: Compulsive hair pulling
- Excoriation disorder: Compulsive skin picking
OCD Features
People with OCD experience:
- Obsessions: Intrusive, unwanted thoughts, images, or urges that cause anxiety (fear of contamination, harm, symmetry)
- Compulsions: Repetitive behaviors or mental acts performed to reduce anxiety (excessive checking, washing, counting, arranging)
Most people with OCD recognize their thoughts as irrational yet feel compelled to perform rituals anyway. These behaviors can consume hours each day.
Symptoms often begin in childhood, adolescence, or early adulthood. Research suggests earlier onset is more common in males.
Treatment
- Exposure and response prevention (ERP), a specialized form of CBT
- SSRIs at higher doses than typically used for depression
- Family education to avoid reinforcing compulsions
- Structured support and sometimes more intensive interventions for severe cases
7. Eating Disorders
Eating disorders are serious mental health conditions where food, body weight, and shape become overwhelming preoccupations that harm both physical health and emotional well-being.
Main Diagnoses
| Disorder | Key Features |
|---|---|
| Anorexia nervosa | Severe restriction, significantly low body weight, intense fear of gaining weight |
| Bulimia nervosa | Binge eating followed by compensatory behaviors (vomiting, laxatives, excessive exercise) |
| Binge eating disorder | Recurrent binges without regular purging, marked distress |
Around 16 million people worldwide were living with eating disorders in 2021. Many cases begin in adolescence or early adulthood.
Medical Risks
Common eating disorders carry severe physical consequences:
- Malnutrition and vitamin deficiencies
- Electrolyte imbalances (can cause cardiac arrest)
- Organ damage
- Dental erosion (from purging)
- Bone loss
- Death (anorexia nervosa has one of the highest mortality rates of any mental illness)
Treatment Approaches
- Family-based therapy (especially for adolescents with anorexia)
- CBT-E (enhanced cognitive behavioral therapy)
- Nutritional rehabilitation
- Medical monitoring
- Inpatient or residential care for severe cases
Early intervention dramatically improves outcomes for eating disorders.
8. Personality Disorders
Personality disorders involve enduring patterns of inner experience and behavior that deviate markedly from cultural expectations. These patterns are inflexible, begin in adolescence or early adulthood, and cause long-term problems in self-image and relationships.
DSM-5 Clusters
| Cluster | Characteristics | Examples |
|---|---|---|
| Cluster A | Odd, eccentric | Paranoid personality disorder, schizoid, schizotypal |
| Cluster B | Dramatic, emotional, erratic | Borderline personality disorder, antisocial, histrionic, narcissistic |
| Cluster C | Anxious, fearful | Avoidant, dependent, obsessive-compulsive personality disorder |
Approximately 10% of people may meet criteria for at least one personality disorder at some point in their lives.
Specific Examples
- Borderline personality disorder: Emotional instability, fear of abandonment, unstable relationships, self harm, impulsive behavior
- Antisocial personality disorder: Disregard for others’ rights, law-breaking, lack of remorse
- Narcissistic personality disorder: Grandiosity, need for admiration, lack of empathy
- Avoidant personality disorder: Social inhibition, feelings of inadequacy, hypersensitivity to criticism
Personality disorders frequently overlap with other mental disorders like depression, anxiety, and substance use, complicating both diagnosis and treatment.
Treatment and Support
- Long-term psychotherapy (dialectical behavior therapy for BPD, schema therapy)
- Skills training for emotional regulation
- Crisis planning and safety strategies
- Support for families and carers
- Treatment of co-occurring conditions
9. Neurodevelopmental Disorders
Neurodevelopmental disorders appear early in development, often before school age. They involve difficulties in learning, behavior, or social communication that persist into adulthood for many people.
Key Conditions
- Intellectual disability: Significant limitations in intellectual functioning and adaptive behavior
- Autism spectrum disorder (ASD): Challenges in social communication, restricted or repetitive behaviors, sensory sensitivities
- Attention deficit hyperactivity disorder (ADHD): Persistent inattention, hyperactivity, and impulsivity
- Specific learning disorders: Difficulties with reading (dyslexia), mathematics, or written expression
Core Features
ADHD symptoms:
- Difficulty sustaining attention
- Easily distracted
- Hyperactivity and restlessness
- Impulsive decision-making
- Difficulty with organization
Autism spectrum disorder features:
- Challenges in social communication and interaction
- Restricted, repetitive patterns of behavior or interests
- Sensory sensitivities
- Variable presentation from mild to severe
ADHD is diagnosed in roughly 8-10% of school-aged children in the United States, with many continuing to have symptoms into adulthood.
Interventions
- Behavioral therapy and parent training
- Educational support plans (IEPs, 504 plans)
- Occupational and speech therapy
- Social skills training
- Stimulant or non-stimulant medications for ADHD (carefully monitored)
10. Substance-Related and Addictive Disorders
Modern diagnostic systems classify substance use disorders and certain behavioral addictions as mental disorders because they alter brain circuits involved in reward, decision-making, and self-control.
What’s Included
- Alcohol use disorder
- Opioid use disorder
- Stimulant use disorder
- Cannabis use disorder
- Tobacco use disorder
- Gambling disorder (behavioral addiction)
Pattern of Problematic Use
| Feature | Description |
|---|---|
| Craving | Strong urges to use the substance |
| Tolerance | Needing more to achieve the same effect |
| Withdrawal | Physical and psychological symptoms when stopping |
| Loss of control | Failed attempts to cut down or quit |
| Neglect | Abandoning responsibilities at work, school, or home |
| Continued use despite harm | Using even when it damages health, relationships, or finances |
The DSM-5 recognizes substance use disorder as a mental health diagnosis. Many substance abusers also live with co-occurring conditions like depression, anxiety, PTSD, or bipolar disorder.
Serious Consequences
- Overdose and death
- Accidents and injuries
- Legal problems
- Infections (HIV, hepatitis)
- Long-term organ damage
- Relationship and family breakdown
Treatment Options
- Medically supervised detoxification
- Medication-assisted treatment (buprenorphine, methadone for opioids; naltrexone for alcohol)
- Individual and group therapy
- Mutual-help groups (AA, NA, SMART Recovery)
- Integrated care for co-occurring mental illnesses
Why These 10 Types Matter (Impact and Risk Factors)
These 10 categories collectively represent the vast majority of mental health conditions that affect people worldwide. Their impact extends beyond the individual to families, workplaces, schools, and communities.
Key Risk Factors
Understanding what increases risk can guide prevention efforts:
- Genetic predisposition: Family history of mental disorders
- Childhood adversity: Abuse, neglect, household violence
- Chronic stress: Ongoing financial problems, work stress, caregiving burden
- Poverty and discrimination: Limited resources and social marginalization
- Physical illness: Chronic medical conditions
- Substance use: Drug and alcohol misuse
Protective Factors
Factors that reduce risk and support recovery:
- Stable, supportive caregiving in childhood
- Strong social support networks
- Access to education and healthcare
- Effective coping skills
- Safe communities
- Early intervention when problems arise
Many factors combine to determine who develops a mental disorder. Importantly, many mental disorders start before age 25, highlighting the importance of early recognition in children, teenagers, and young adults.
The hopeful reality: early help reduces severity, shortens episodes, and improves long-term outcomes.
Diagnosis, Treatment, and Getting Help
How Diagnosis Works
Mental health professionals diagnose disorders using:
- Clinical interviews and observation
- Medical exams (to rule out physical causes)
- Psychological questionnaires and assessments
- Criteria from the DSM-5-TR or ICD-11 (the Statistical Manual used by clinicians)
There are no single medical tests (like blood tests or brain scans) that definitively diagnose most mental disorders. Diagnosis relies on trained clinical judgment.
Treatment Categories
| Type | Examples |
|---|---|
| Psychotherapy | CBT, dialectical behavior therapy, interpersonal therapy, exposure therapy |
| Medication | Antidepressants, mood stabilizers, antipsychotics, anti-anxiety medications |
| Lifestyle changes | Regular exercise, adequate sleep, reduced substance use, stress management |
| Peer support | Support groups, peer specialists |
| Intensive services | Day programs, partial hospitalization, inpatient care |
Treatment is personalized. What works for depression may differ significantly from what’s needed for schizophrenia, eating disorders, or PTSD. Many people benefit from combining multiple approaches.
Where to Start
If you’re unsure where to seek help, consider:
- Primary care doctor (can screen and provide referrals)
- Community mental health clinic
- School counselor or university counseling center
- Employee assistance program
- Mental health services through insurance
Crisis Note: If you or someone you know is at immediate risk of self-harm or harming others, contact emergency services or a local crisis hotline right away. This is not something to wait out.
Frequently Asked
Questions about Mental Health Disorders
What are the serious mental disorders?
Serious Mental Illnesses (SMI) are conditions that significantly interfere with daily functioning, relationships, or the ability to work or care for oneself.
Common examples include:
-
Schizophrenia
-
Bipolar I Disorder
-
Major Depressive Disorder (severe or recurrent)
-
Schizoaffective Disorder
-
Severe Post-Traumatic Stress Disorder (PTSD)
The National Institute of Mental Health (NIMH) and Substance Abuse and Mental Health Services Administration (SAMHSA) classify these as SMIs due to their intensity and need for ongoing treatment.
What are chronic mental disorders?
Chronic mental disorders are conditions that tend to be long-term or recurring, though symptoms can improve or go into remission.
Examples include:
-
Bipolar Disorder
-
Schizophrenia
-
Major Depressive Disorder
-
Generalized Anxiety Disorder
-
Obsessive-Compulsive Disorder (OCD)
-
Post-Traumatic Stress Disorder (PTSD)
Important note:
“Chronic” does not mean untreatable. According to NIMH, many people live stable, productive lives with proper care.
What are the 20 types of mental disorders?
Below are 20 commonly recognized mental disorders, based on categories in the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders):
-
Major Depressive Disorder (MDD)
-
Bipolar I Disorder
-
Bipolar II Disorder
-
Schizophrenia
-
Schizoaffective Disorder
-
Generalized Anxiety Disorder (GAD)
-
Panic Disorder
-
Social Anxiety Disorder
-
Post-Traumatic Stress Disorder (PTSD)
-
Obsessive-Compulsive Disorder (OCD)
-
Attention-Deficit/Hyperactivity Disorder (ADHD)
-
Autism Spectrum Disorder (ASD)
-
Borderline Personality Disorder (BPD)
-
Antisocial Personality Disorder
-
Avoidant Personality Disorder
-
Eating Disorders (e.g., anorexia, bulimia)
-
Substance Use Disorders
-
Dissociative Identity Disorder
-
Insomnia Disorder
-
Somatic Symptom Disorder
How do you know if you have a mental illness?
You may have a mental health condition if symptoms:
-
Last weeks or months
-
Interfere with work, school, or relationships
-
Affect mood, thinking, behavior, or perception
-
Don’t improve with rest or stress reduction
Common signs include:
-
Persistent sadness or anxiety
-
Extreme mood changes
-
Withdrawal from others
-
Changes in sleep, appetite, or energy
-
Difficulty functioning day to day
Only a licensed mental health professional can diagnose a mental disorder using DSM-5 criteria.
What’s the difference between having a mental disorder and just feeling stressed or sad?
Feeling stressed, sad, or overwhelmed is a normal human response to life events.
A mental disorder is different because:
-
Symptoms are more intense
-
They last longer
-
They impair daily functioning
-
They often require professional treatment
Key distinction:
Stress is situational and temporary; mental disorders are persistent patterns involving brain function, behavior, and emotional regulation.
Can mental disorders be cured, or are they lifelong?
Some mental disorders can go into full remission, while others require ongoing management.
-
Conditions like depression or anxiety may fully resolve
-
Disorders like bipolar disorder or schizophrenia are usually lifelong but highly manageable
The World Health Organization (WHO) and NIMH emphasize that recovery means living well, not necessarily being symptom-free forever.
How common is it to have more than one mental disorder?
Very common.
According to NIMH:
-
About 50% of people with a mental disorder have at least one co-occurring condition
-
This is known as comorbidity or co-occurring disorders
Common combinations include:
-
Depression + anxiety
-
PTSD + substance use disorder
-
Bipolar disorder + anxiety disorder
How can I help a loved one who might be struggling with a mental health condition?
You can help by:
-
Listening without judgment
-
Encouraging professional help gently
-
Learning about their condition
-
Avoiding minimizing or dismissing their experience
-
Supporting treatment and healthy routines
Helpful resources include:
- Legacy Healing Center Helpline (1-888-534-2295)
-
NAMI (National Alliance on Mental Illness)
-
SAMHSA’s National Helpline (1-800-662-HELP)
Important reminder:
You can support someone—but you cannot diagnose or “fix” them on your own.