Effective Treatment Options for Drug and Alcohol Use Disorders (SUD & AUD)
-
By: Alex Herrera
-
Editor: Phyllis Rodriguez, PMHNP-BC
-
Clinical Reviewer: Dr. Ash Bhatt, MD, MRO
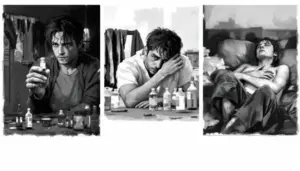
Substance use disorders affect more than 48 million Americans each year, yet fewer than 1 in 20 people who need treatment actually receive it. In fact, many people delay seeking help because they’re unsure whether their situation is “serious enough” or because they don’t fully understand what treatment actually involves.
Effective drug and alcohol abuse treatment goes beyond stopping substance use. It addresses physical dependence while also treating the emotional and mental health challenges that often fuel addiction in the first place. This guide explains proven treatment options, how to choose the right level of care, and what to expect when starting treatment, so you can take the next step with clarity and confidence.


The Key Takeaways:1. Addiction is a medical condition 2. Recovery works best with combined treatment 3. Healing continues beyond rehab |
What Drug and Alcohol Use Disorders Really Are
Drug and alcohol use disorders are chronic, progressive conditions that affect both brain function and behavior. Over time, repeated substance use changes how the brain processes reward, stress, and decision-making, making it increasingly difficult to stop without structured support. The National Institute on Drug Abuse (NIDA) explains that these changes are not temporary; they alter brain pathways in ways that reinforce continued use, even when someone wants to quit.
Substance use disorder (SUD) is a broad medical term that includes several conditions, most commonly:
- Alcohol Use Disorder (AUD)
- Opioid Use Disorder (OUD)
- Dependence on substances such as stimulants, sedatives, or hallucinogens
What makes these disorders complex is that they rarely develop for just one reason. Genetics, trauma, untreated mental health conditions, environmental exposure, and prolonged substance use often interact over time. As the disorder progresses, individuals may notice increasing tolerance, stronger cravings, disrupted sleep, mood changes, or continued use despite clear negative consequences.
We view addiction as a whole-person condition, not a single symptom to be corrected. Effective treatment addresses physical dependence alongside emotional health, behavioral patterns, and underlying mental health concerns, because lasting recovery requires all of these pieces to be treated together.
Understanding the Diagnosis of Substance Use Disorders
Accurate diagnosis is the foundation of effective treatment. The DSM-5 diagnostic criteria help identify patterns such as loss of control, increased tolerance, withdrawal symptoms, and continued use despite physical, emotional, or social harm. A comprehensive assessment often includes a combination of:
- Clinical interviews and substance use history
- Screening for anxiety, depression, PTSD, and other mental health disorders
- Medical evaluations or lab testing when needed
Identifying co-occurring mental health conditions is a critical part of this process. The American Psychiatric Association (APA) and SAMHSA emphasize that untreated mental health disorders significantly increase the risk of relapse. By addressing these conditions early, it is easy to create a treatment plan that targets every contributing factor, rather than focusing on substance use alone.
Treatment Options for Drug and Alcohol Abuse
What works for one person may not work for another, which is why effective treatment must be flexible, personalized, and responsive to both substance use severity and mental health history. The most successful outcomes come from combining medical care, therapy, and long-term support, rather than relying on any one approach alone.
Our treatment approach follows a structured continuum:
- Stabilization through detox and medical oversight
- Comprehensive assessment and treatment planning
- Core treatment through residential or outpatient care
- Skill-building, relapse prevention, and aftercare planning
Given below are the core components of treatment, and each phase builds on the last, creating a clear and supportive path forward.
1. Medications for Substance Use Disorders and Alcohol Treatment
Medication-Assisted Treatment (MAT) is an evidence-based option for treating both alcohol and opioid use disorders. When used appropriately, MAT helps regulate brain chemistry, reduce cravings, and lower the risk of relapse.
Depending on clinical needs, treatment may include FDA-approved medications such as:
- Naltrexone, which reduces alcohol cravings and blocks rewarding effects
- Acamprosate, which supports long-term abstinence in alcohol use disorder
- Disulfiram, which discourages drinking by causing adverse physical reactions
- Buprenorphine or Methadone, which reduce opioid cravings and withdrawal symptoms
Research supported by SAMHSA and NIDA shows that MAT significantly improves treatment retention and recovery outcomes when combined with therapy and behavioral support.
2. Behavioral Therapies for Addiction and Mental Health
Medication alone is rarely enough. Therapy helps individuals understand the patterns that drive substance use and develop healthier coping strategies. We use evidence-based behavioral therapies tailored to each person’s needs, which include:
- Cognitive Behavioral Therapy (CBT) to address thought-behavior cycles
- Motivational interviewing to strengthen commitment to change
- Individual therapy for trauma and emotional regulation
- Group therapy for accountability and peer support
- Family and couples therapy to repair relationships
Behavioral therapies are central to long-term recovery and mental health stability.
3. Residential Treatment Programs for Drug Addiction
Residential treatment provides a structured, immersive environment with 24/7 clinical support. This level of care is often recommended for individuals with severe substance use disorders, repeated relapses, or co-occurring mental health conditions who require close monitoring. Residential treatment typically includes:
- Medically supervised detox
- Individual, group, and family therapy
- Psychiatric care and medication management
- Structured daily routines and wellness activities
- Relapse prevention and life-skills development
4. Outpatient Treatment Options
Outpatient treatment allows individuals to receive structured care while continuing work, school, or family responsibilities. The level of intensity depends on clinical needs and recovery progress. Outpatient options may include:
- Partial Hospitalization Programs (PHP)
- Intensive Outpatient Programs (IOP)
- Traditional outpatient therapy (OP)
Outpatient treatment is commonly used as a step-down from residential care or for individuals with stable living environments and strong support systems.
5. Alternative and Complementary Therapies
In addition to clinical treatment, incorporating complementary therapies supports emotional regulation, stress reduction, and overall well-being. These approaches help individuals reconnect with themselves and stay engaged in the recovery process.
Complementary therapies may include yoga and meditation, art or music therapy, mindfulness practices, and nature-based or experiential activities. While these therapies are not a replacement for medical or behavioral care, they enhance balance, self-awareness, and emotional resilience.

Traveling for treatment?
You Don’t Have to Do This Alone
Speak confidentially with a Legacy Healing Center specialist or check your insurance in minutes. Both options are private, free, and focused on helping you start healing.
Talk to a Treatment Specialist
Verify Your Insurance in 2 Minutes
You Don’t Have to Do This Alone
Speak confidentially with a Legacy Healing Center specialist or check your insurance in minutes. Both options are private, free, and focused on helping you start healing.

Talk to a Treatment Specialist
Get immediate, confidential guidance on your treatment options and insurance.
24/7 Admissions | 100% Private

Check Your Insurance in 2 Minutes
Answer a few quick questions to see if you may qualify for treatment.
Traveling for treatment?
Our team can arrange flights and transportation for you.
Managing Withdrawal Symptoms Safely
One of the biggest concerns people have is what happens when they stop using drugs or alcohol. Withdrawal is often the first step toward recovery, but it can also be physically and emotionally challenging.
Withdrawal symptoms can range from mild discomfort to serious medical complications. Some people experience anxiety, agitation, or difficulty sleeping, while others may develop tremors, nausea, confusion, or hallucinations. In more severe cases, particularly with alcohol use, withdrawal can involve seizures and requires immediate medical attention.
That’s why we provide medically supervised detox. This level of care allows us to monitor symptoms closely, manage discomfort, and reduce complications while helping individuals stabilize safely before moving into the next phase of treatment.
Ongoing Support and Research-Driven Care in Recovery
Recovery doesn’t end when formal treatment does. Long-term healing is strongest when individuals remain connected to supportive people and continue care informed by current research. Sustainable recovery relies on both human connection and evidence-based clinical practices.
Ongoing recovery support often includes:
- Family counseling and education to strengthen understanding and communication
- Peer support groups such as Alcoholics Anonymous (AA) or Narcotics Anonymous (NA)
- Alumni programs and structured follow-up care
- Continued mental health check-ins to address stress and relapse risk
At the same time, addiction treatment continues to evolve through research supported by organizations such as NIDA, NIH, and SAMHSA. Advances in medications for cravings and withdrawal, behavioral therapies, and trauma-informed approaches help improve long-term outcomes. By integrating these research-driven practices, treatment remains current, effective, and responsive to individual needs.
Preparing for AUD or SUD Treatment?
If you’re struggling with alcohol use, drug addiction, or co-occurring mental health challenges, help is available.
Our admissions team guides each person through the process with discretion, clarity, and compassion.
Call today to speak with a treatment provider, verify insurance, and take the next step toward recovery.
Frequently Asked
Questions about Drug and Alcohol Abuse Treatment
How long does drug and alcohol abuse treatment last?
The duration of drug and alcohol abuse treatment depends on the severity of the addiction and individual needs. Detox typically lasts 3–7 days, residential programs 30–90 days, and outpatient treatment or ongoing therapy can continue for months to support lasting recovery.
Can treatment address co-occurring mental health conditions?
Yes. Effective drug and alcohol abuse treatment at Legacy Healing Center includes integrated care for co-occurring mental health conditions such as anxiety, depression, PTSD, or bipolar disorder. Addressing both addiction and mental health improves stability, reduces relapse risk, and enhances long-term recovery outcomes.
Is outpatient treatment effective for alcohol or drug addiction?
Outpatient drug and alcohol treatment programs allow clients to continue work, school, or family responsibilities while receiving therapy, support groups, and mental health services. This step-down approach is ideal for early recovery or transitioning from residential care, ensuring ongoing support and relapse prevention.
Does Legacy Healing Center provide support for families?
Yes. Addiction treatment services at Legacy include family counseling and therapist-guided sessions. Families learn how to support their loved ones, rebuild trust, and actively participate in recovery. Strong family involvement improves accountability, reduces relapse risk, and fosters a healthier long-term environment for recovery.
Can I travel safely to Legacy Healing Center for treatment?
Absolutely. Our complimentary Travel Concierge Service helps coordinate flights, transportation, and accommodations for clients seeking drug and alcohol rehab. This ensures a smooth, stress-free transition to treatment, allowing you to focus entirely on recovery without logistical worries.



 By:
By:
 Editor:
Editor:
 Clinical Reviewer:
Clinical Reviewer: