Bipolar Disorder: Complete Guide to Understanding, Managing, and Living with Manic-Depressive Illness
-
 By:
Valerie Puffenberger, PMHNP-BC
By:
Valerie Puffenberger, PMHNP-BC
-
 Editor:
Phyllis Rodriguez, PMHNP-BC
Editor:
Phyllis Rodriguez, PMHNP-BC
-
 Clinical Reviewer:
Dr. Ash Bhatt, MD, MRO
Clinical Reviewer:
Dr. Ash Bhatt, MD, MRO
What is Bipolar Disorder and Why It Matters
Bipolar disorder is a lifelong illness and mental health condition affecting 1-5% of the global population, characterized by extreme mood swings between manic highs and depressive lows. It is also known as manic depressive disorder. In this comprehensive guide, you’ll learn what bipolar disorder is, how to recognize symptoms, and evidence-based treatment for bipolar disorder.
Bipolar disorder can start at any age, but it is usually diagnosed in the teenage years or early 20s, with the average age of onset in the mid-20s.
People with bipolar disorder experience dramatic shifts in mood, energy, and activity levels that significantly impact daily functioning. People with bipolar disorder often experience a decline in cognitive functioning during or possibly before their first episode. Unlike normal mood changes, bipolar episodes last for days or weeks and can severely disrupt relationships, work performance, and overall quality of life. Bipolar disorder is associated with higher rates of unemployment and difficulty keeping a job.
This guide covers:
- Types of bipolar disorder and diagnostic criteria
- The process of how bipolar disorder is diagnosed
- Symptom recognition for manic and depressive episodes
- Evidence-based treatment options and management strategies
- Practical lifestyle approaches for long-term stability
- Real-world case studies and frequently asked questions
Whether you’re seeking information for yourself, a loved one, or professional knowledge, this resource provides immediate confirmation of search intent for patients, families, and healthcare seekers.
Understanding Bipolar Disorder: Key Concepts and Definitions
Core Definitions
Bipolar disorder, also known as manic depressive illness, is a chronic mood disorder characterized by alternating episodes of mania or hypomania and depression, known as manic or depressive episodes. This disorder is also historically referred to as manic depressive disorder. These mood episodes represent significant changes from a person’s mood baseline and involve extreme mood episodes that differ markedly from a person’s typical mood and behavior.
Key terminology includes:
- Mood episodes: Distinct periods of abnormal mood lasting days to weeks, including manic or depressive episodes
- Euthymia: Stable periods between mood episodes when symptoms are minimal; people with bipolar disorder often have periods of neutral mood between episodes
- Manic depression: Historical term for what we now call bipolar disorder, highlighting mood swings, behavioral changes, and energy fluctuations
- Manic and hypomanic episodes: Periods of abnormally elevated, expansive, or irritable mood; manic episodes are more severe, may require hospitalization, and last at least 7 days, while hypomanic episodes are less severe and last at least 4 days
- Manic or hypomanic episodes: Key features of bipolar disorder, characterized by elevated mood, increased activity or energy, and other symptoms; their occurrence and severity are important for diagnosis
- Bipolar symptoms: The collection of emotional, behavioral, and physical changes during episodes
Pro Tip: Distinguish between normal mood changes and clinical bipolar episodes. While everyone experiences ups and downs, bipolar disorder involves mood episodes lasting days to weeks with significant functional impairment, not typical daily mood fluctuations.
Lasting Results: Kevin regained self-respect and learned practical tools to stay grounded in recovery. He has new friends and a new lease on life.

Types and Classifications
The Diagnostic and Statistical Manual (DSM-5) and ICD-11 classify bipolar disorders into several distinct types:
- Bipolar I Disorder requires at least one manic episode lasting at least one week or requiring hospitalization. Manic episodes in bipolar I may include psychosis. People with bipolar I often experience severe manic episodes, along with major depressive episodes.
- Bipolar II Disorder involves hypomanic episodes lasting at least four consecutive days, plus major depressive episodes. Bipolar II typically does not include psychosis. Individuals with bipolar II disorder often first seek treatment due to their depressive episodes, as hypomanic episodes can feel pleasurable. While hypomanic episodes are less severe than full blown manic episodes, bipolar II disorder often causes more functional impairment due to frequent depressive symptoms.
- Cyclothymic Disorder presents as milder mood swings over 2+ years, with hypomanic and depressive symptoms that don’t meet full criteria for major mood episodes. This milder form can still significantly impact daily life and may progress to bipolar I or II disorder.
- Rapid cycling is a course specifier for bipolar disorder, defined as having four or more mood episodes (manic, hypomanic, or depressive) within a year. Rapid cycling is clinically significant because it can complicate treatment and is associated with a more challenging prognosis.
Severe depression can occur as a phase of bipolar disorder, especially following hypomanic episodes, and can have a significant impact on mood and daily functioning. Bipolar depression is a specific phase that requires targeted treatment, often with medications approved for depressive episodes in bipolar disorder, such as certain atypical antipsychotics and mood stabilizers.
Prevalence estimates of bipolar disorder in children and young adults range from 0.6% to 15%, depending on settings and methods. A meta-analysis estimated that about 1.8% of people between the ages of seven and 21 have bipolar disorder. The incidence of bipolar disorder is similar in men and women, and it is thought to occur at a similar frequency in boys and girls.
These classifications connect directly to DSM-5 diagnostic criteria and ICD-11 classifications, ensuring standardized diagnosis across mental health professionals worldwide.
Why Bipolar Disorder is Important in Mental Health
Bipolar disorder represents one of the most significant mental health conditions globally. According to the World Health Organization, bipolar disorder ranks as the 6th leading cause of disability worldwide, highlighting its substantial impact on individuals and society.
The statistical reality is sobering: people with bipolar disorder face a 15-20% suicide rate, with 34% attempting suicide during their lifetime. This mental illness carries profound risks that extend far beyond mood symptoms, affecting every aspect of a person’s life.
Economic costs reach staggering levels, with $202 billion in annual costs in the U.S. alone (2015 data). These expenses encompass direct medical care, lost productivity, and indirect costs affecting families and communities.
Perhaps most concerning is the average 8-year delay between symptom onset and proper treatment. Early intervention proves crucial for preventing severe episodes, reducing suicide risk, and maintaining functional capacity. Mental health specialists emphasize that prompt recognition and treatment of bipolar disorder symptoms can dramatically improve long-term outcomes and quality of life.
Bipolar Disorder Types Comparison Table
| Feature | Bipolar I Disorder | Bipolar II Disorder | Cyclothymic Disorder |
|---|---|---|---|
| Manic Episodes | At least one full manic episode lasting at least 1 week | No full manic episodes | Hypomanic symptoms only |
| Hypomanic Episodes | May occur; must last at least 4 consecutive days | Required (at least 4 consecutive days) | Required (multiple episodes, at least 4 consecutive days each) |
| Depressive Episodes | Major depressive episodes common | At least one major depressive episode | Mild depressive symptoms |
| Bipolar Depression | Present; depressive episodes can be severe and require targeted treatment | Present; depressive episodes are significant and often more frequent | Mild depressive symptoms, not meeting criteria for major bipolar depression |
| Rapid Cycling | Can occur (≥4 mood episodes/year); associated with more complex course and treatment challenges | Can occur (≥4 mood episodes/year); may complicate management | Rare |
| Hospitalization | Often required during severe manic episodes | Rarely required | Not typically required |
| Functional Impairment | Severe during acute episodes | Often chronic due to frequent depression | Persistent but milder |
| Age of Onset | Typically around age 18 | Typically around age 22 | Often begins in adolescence |
| Psychotic Symptoms | May occur during severe episodes | Rare | Does not occur |
| Episode Duration | Weeks to months | Days to weeks | Persistent fluctuations |
Step-by-Step Guide to Recognizing and Managing Bipolar Disorder
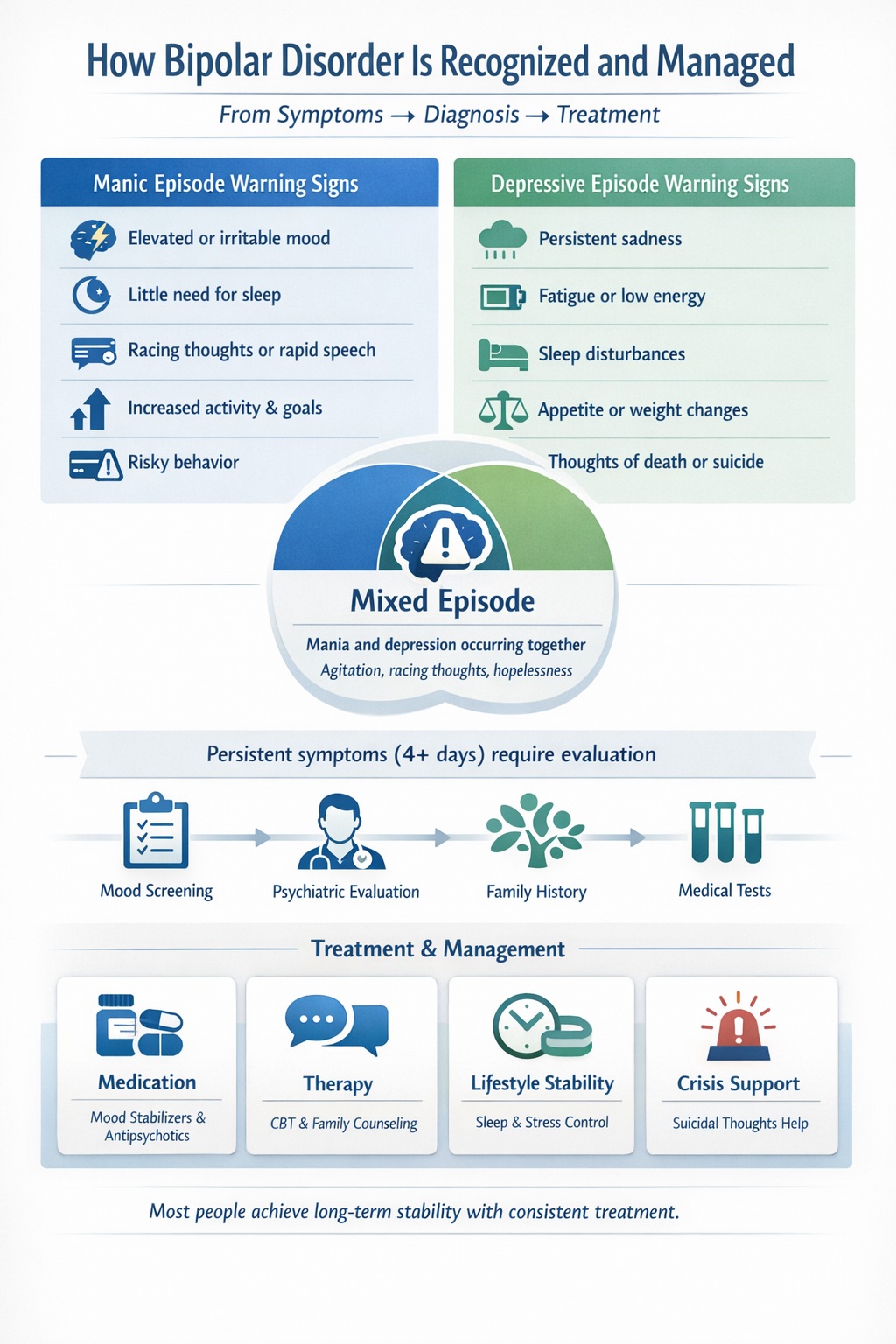
Step 1: Identify Warning Signs and Symptoms
Manic Episode Checklist:
When looking for symptoms of bipolar disorder, it is important to recognize the distinct phases known as manic or depressive episodes.
- Elevated, euphoric, or irritable mood lasting at least 7 days (part of a manic episode)
- Decreased sleep need (functioning on 3+ hours without fatigue)
- Grandiosity or inflated self-esteem
- Racing thoughts and rapid speech
- Distractibility and poor judgment
- Increased goal-directed activity or psychomotor agitation
- Risky behavior (excessive spending, sexual indiscretions, substance abuse)
Depressive Episode Indicators:
These symptoms of bipolar disorder occur during a depressive episode.
- Persistent sadness or depressed mood lasting 2+ weeks
- Loss of interest or pleasure in activities
- Significant fatigue or loss of energy
- Sleep disturbances (insomnia or hypersomnia)
- Appetite changes and weight fluctuations
- Feelings of worthlessness or inappropriate guilt
- Concentration difficulties
- Suicidal ideation or thoughts of death
Mixed Episode Recognition:
Some people experience mixed episodes with simultaneous manic and depressive symptoms, presenting as agitated depression or dysphoric mania.
Step 2: Seek Professional Diagnosis
Contact healthcare providers when persistent mood changes last 4+ days and significantly impact daily functioning. Early professional evaluation is essential to have bipolar disorder diagnosed and prevents progression to more severe episodes.
Diagnostic Tools:
- Mood Disorder Questionnaire (MDQ) for initial screening
- Comprehensive clinical interviews with mental health specialists
- Family history assessment (bipolar disorder has strong genetic components)
- Medical evaluation to rule out other conditions
It is important to differentiate bipolar disorder from other mental disorders, as symptoms can overlap with conditions such as anxiety disorders, ADHD, or substance use disorders. A thorough mental health evaluation must exclude medical conditions like thyroid disorders, neurological conditions, or substance use disorders that can mimic bipolar symptoms. Mental health professionals use specific criteria to diagnose bipolar disorder accurately.
Step 3: Implement Treatment Plan
Medication Options:
- Pharmacological treatment is the cornerstone of managing bipolar disorder, with mood stabilizers such as lithium (FDA-approved for children), valproate, and carbamazepine being the mainstay.
- Atypical antipsychotics: Quetiapine, olanzapine, aripiprazole for acute episodes
- Combination therapy: Often required for optimal symptom control
- Antidepressants are used cautiously in bipolar disorder due to the risk of triggering manic episodes.
- In some cases, electroconvulsive therapy (ECT) may be considered, especially when medication response is inadequate.
Psychotherapy Approaches:
- Cognitive Behavioral Therapy (CBT) for mood regulation skills
- Family-focused therapy to improve communication and support
- Interpersonal and social rhythm therapy for routine stabilization
- Talk therapy for ongoing symptom management
Crisis Management:
Seek emergency help immediately for suicidal thoughts, severe mania with dangerous behavior, or psychotic symptoms. Contact crisis hotlines (988 in the U.S.) or emergency services when safety is at risk.
Common Mistakes to Avoid
- Mistake 1: Stopping medication during stable periods. Over 75% of patients have medication adherence issues, often discontinuing treatment when feeling better. This leads to rapid relapse and potentially more severe episodes. Ongoing treatment is essential to prevent bipolar disorder from progressing or worsening, as early intervention and consistent management help reduce the risk of future episodes.
- Mistake 2: Misinterpreting hypomania as just “feeling good” and avoiding treatment. Hypomania symptoms may seem positive initially, but they signal an underlying mood disorder requiring professional attention.
- Mistake 3: Using prescribed antidepressants alone without mood stabilizers. Antidepressants can trigger manic episodes in people with bipolar disorder, making proper diagnosis crucial before treatment.
Pro Tip: Maintain consistent sleep schedules as sleep deprivation triggers mania in 30% of patients. Regular sleep patterns serve as both treatment and prevention for bipolar episodes.
Real-Life Case Study: Managing Bipolar II Disorder
Case Study:
Sarah, a 28-year-old marketing professional, was diagnosed with bipolar II disorder after years of misdiagnosis and unsuccessful treatment for major depression.
Starting Situation: Sarah experienced recurrent depressive episodes lasting months, interspersed with brief periods of high productivity and creativity that she and her doctors interpreted as recovery from depression. Her depressive episodes were consistent with bipolar depression, which requires targeted treatment with medications approved specifically for depressive episodes within bipolar disorder. She had been prescribed antidepressants multiple times, which provided temporary relief but often led to increased anxiety and irritability.
Treatment Approach:
- Medication adjustment: Discontinued antidepressants and started lamotrigine (mood stabilizer)
- Cognitive Behavioral Therapy: Weekly sessions focusing on mood monitoring and coping strategies
- Sleep hygiene: Established consistent sleep-wake cycles
- Family education: Involved partner in recognizing early warning signs
- Lifestyle modifications: Regular exercise, stress management, limited alcohol use
Outcomes: 18-month follow-up showed remarkable improvement:
- 70% reduction in depressive episodes (from 6 episodes per year to 2)
- Improved work functioning with consistent performance ratings
- Better relationship stability with enhanced communication skills
- Medication adherence rate of 95% with minimal side effects
Before/After Assessment:
- Work productivity: 60% → 90%
- Relationship satisfaction: 4/10 → 8/10
- Quality of life score: 35/100 → 78/100
- Hospitalization days: 14 days → 0 days
Co-occurring Conditions: When Bipolar Disorder Meets Other Mental Health Challenges
If you’re living with bipolar disorder, you may also navigate other mental health challenges alongside your primary condition — what we call co-occurring conditions. This isn’t uncommon, and you’re not alone in this experience. Research shows that about half of people on your journey will face at least one additional mental health challenge during their lifetime. You might recognize anxiety disorders, substance use concerns, or attention-deficit/hyperactivity disorder (ADHD) as part of your story. These overlapping experiences can make your path to wellness more complex, as symptoms may mirror each other or create confusion in your healing process.
For instance, anxiety can intensify your mood fluctuations or make depressive periods feel more persistent, while substance use might trigger or amplify manic episodes in your experience. Sometimes, medications prescribed for other conditions — like certain antidepressants — can actually provoke manic symptoms when you have bipolar disorder. But here’s what gives us hope: understanding these complexities means your care team can develop a comprehensive treatment plan that honors every aspect of your mental health journey. This thoughtful approach involves careful coordination between your healthcare providers, gentle monitoring of your progress, and mindful selection of treatments that work together rather than against each other. By embracing this holistic path, you can achieve better symptom management and discover the lasting mental wellness you deserve.
Lifestyle Changes and Self-Care for Bipolar Disorder
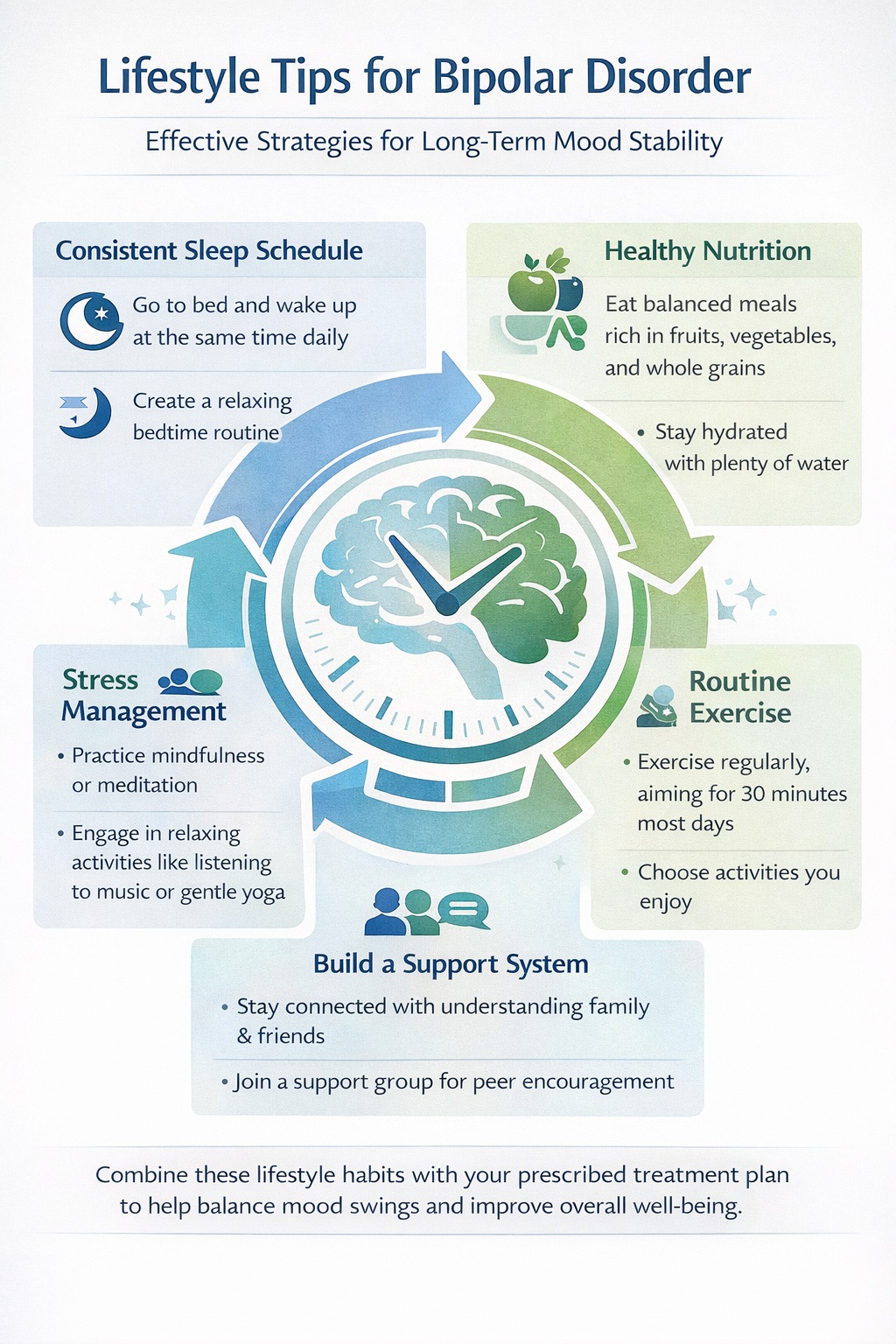
Making positive changes in your daily life and embracing gentle self-care can become your most powerful allies in managing bipolar disorder and nurturing your long-term mental wellness. When you establish a steady daily rhythm—especially honoring consistent sleep and wake times—you’re creating a foundation that helps stabilize your mood and shields you from both the highs of mania and the depths of depression. Nourishing your body with wholesome foods and moving it regularly becomes more than routine—it’s your pathway to sustained energy and emotional harmony.
Learning to navigate stress becomes another cornerstone of your healing journey. Practices like meditation, yoga, and mindful breathing can gently ease the weight of anxiety and lift the shadows of depression, making your daily challenges feel more manageable. When you set goals that honor where you are today, practice kindness toward yourself, and surround yourself with a circle of support—whether through cherished friends, family, or others who understand your path—you’re building the resilience that will carry you through both storms and sunshine.
Your partnership with a mental health professional becomes the compass for your unique healing journey. Together, you’ll craft a personalized plan that honors your individual needs and dreams, creating a roadmap designed to prevent setbacks and nurture lasting stability. By weaving self-care into your treatment plan, you’re not just managing your mental health—you’re actively transforming your quality of life and writing a story of hope, healing, and renewed possibility.
Suicide and Crisis Management in Bipolar Disorder
If you’re living with bipolar disorder, understanding your unique relationship with suicidal thoughts is one of the most important conversations we can have together. The reality is that your risk may be higher than others, especially during those overwhelming depressive or mixed episodes when hopelessness feels crushing and impulsivity takes over. You’re not alone in this—research shows that up to half of people walking your same journey have faced similar moments of crisis. What matters most is that we recognize these patterns early and build your personal roadmap for staying safe.
Your warning signs might look like talking about death, pulling away from the people who love you, acting recklessly, or experiencing sudden shifts in your emotional landscape. If you’re recognizing yourself in these words right now, please know that reaching out is the most courageous thing you can do. Working with a mental health professional to create your own crisis plan isn’t just paperwork—it’s your lifeline. This plan becomes your guide through the storm, complete with emergency contacts, the coping strategies that work specifically for you, and a carefully chosen list of trusted people who understand your story.
Help is always within reach, and the National Suicide Prevention Lifeline (1-800-273-TALK) is there for you 24/7—no judgment, just immediate support when you need it most. We want you to know that asking for help doesn’t make you weak; it makes you incredibly brave. With the right support system and intervention, you can navigate even the darkest moments safely and continue writing your story of recovery. Healing is possible for everyone—including you.
Creativity and Bipolar Disorder: Myths, Realities, and Insights
The relationship between creativity and bipolar disorder touches something deeply human in all of us — perhaps because we’ve witnessed the profound artistic gifts of so many writers, musicians, and artists who’ve walked this path. When you’re experiencing the heightened energy and emotional intensity that can accompany hypomanic episodes, there’s often a surge in divergent thinking and creative expression that feels almost electric. But here’s what matters most: we must separate the beautiful truth of creative potential from harmful myths.
Living with bipolar disorder means navigating a serious mental health condition that requires real support, real treatment, and real understanding. The romanticized notion of the “tortured artist” does a profound disservice to anyone facing the genuine challenges of severe mood fluctuations and the daily work of mental health management. Your journey with bipolar disorder isn’t about suffering for art — it’s about healing that allows your authentic creative self to flourish. With compassionate care, evidence-based treatment, and ongoing self-advocacy, countless individuals transform their relationship with both their mental health and their creative gifts.
This is where hope lives: in acknowledging that your creative journey can include both struggle and extraordinary achievement. When we embrace accurate, compassionate understanding of mental health and artistic expression, we’re not just reducing stigma — we’re creating space for transformation that benefits everyone. Your creative voice matters, your mental health matters, and with the right support, both can thrive together in ways that inspire not just personal healing, but meaningful contribution to our shared human experience.
Key Takeaways for Living with Bipolar Disorder
Bipolar disorder affects 1-3% of the population and ranks among the most treatable mental health conditions with proper medical care. Understanding that this mental illness involves distinct mood episodes rather than personality flaws represents the first step toward effective management.
Essential takeaways include:
- Early recognition and intervention significantly improve long-term outcomes and prevent severe episodes from developing
- Combination therapy (medication plus psychotherapy) provides the most effective symptom management for treating bipolar disorder
- Strong support systems and lifestyle modifications prove crucial for preventing relapse and maintaining stability
- Consistent treatment adherence remains the most important factor in long-term success
Next steps: Schedule an evaluation with a mental health professional if you’re experiencing persistent mood changes lasting 4+ days. For immediate help with suicidal thoughts or severe symptoms, contact the crisis hotline (988) or emergency services. Remember that bipolar disorder is a medical condition that responds well to treatment, and millions of people with bipolar disorder lead successful, productive lives with proper care.
The journey with bipolar disorder requires patience, commitment, and professional support, but recovery and stability are achievable goals for most people with this mental health condition.
Frequently Asked
Questions about Bipolar Disorder
What is living with bipolar like?
Living with bipolar disorder involves managing recurring mood episodes that range from depressive lows to manic or hypomanic highs. These mood shifts are more intense and longer-lasting than normal emotional changes and can affect energy, sleep, decision-making, relationships, and work.
According to the National Institute of Mental Health (NIMH), many people with bipolar disorder experience periods of stability between episodes, especially when following a consistent treatment plan that includes mood-stabilizing medication, therapy, and routine management.
What is a bipolar 2 person like?
A person with Bipolar II Disorder experiences:
-
Major depressive episodes
-
Hypomanic episodes (a milder form of mania)
Hypomania may look like:
-
Increased energy or productivity
-
Reduced need for sleep
-
Elevated or irritable mood
-
Racing thoughts
Unlike Bipolar I Disorder, Bipolar II does not include full manic episodes or psychosis. The American Psychiatric Association (APA) classifies Bipolar II as equally serious due to the severity and duration of depressive episodes.
What are 5 signs of bipolar disorder?
Common signs of bipolar disorder recognized in the DSM-5 include:
-
Extreme mood swings (highs and lows lasting days or weeks)
-
Changes in sleep patterns (insomnia or sleeping excessively)
-
Impulsive or risky behavior during manic or hypomanic episodes
-
Periods of deep depression, including hopelessness or loss of interest
-
Difficulty concentrating or racing thoughts
Symptoms vary by individual and by whether the person has Bipolar I, Bipolar II, or Cyclothymic Disorder.
Can I live a normal life with bipolar?
Yes. Many people with bipolar disorder live full, stable, and productive lives.
According to NIMH and long-term outcome studies:
-
Consistent treatment
-
Early intervention
-
Medication adherence
-
Psychotherapy (such as Cognitive Behavioral Therapy)
-
Strong support systems
…significantly improve quality of life and reduce episode frequency.
“Normal” life may involve ongoing management, similar to other chronic conditions like diabetes or asthma.
Can bipolar disorder be cured completely?
No. Bipolar disorder cannot currently be cured, but it can be effectively managed long-term.
Medical organizations such as the World Health Organization (WHO) and NIMH classify bipolar disorder as a chronic mood disorder, meaning:
-
Symptoms can go into remission
-
Episodes can be reduced or prevented
-
Lifelong treatment may be needed
Is bipolar disorder hereditary?
Yes. Bipolar disorder has a strong genetic component.
Research cited by NIMH shows:
-
Having a first-degree relative (parent or sibling) with bipolar disorder increases risk
-
Genetics alone do not determine diagnosis—environmental factors also play a role
No single “bipolar gene” exists; risk is polygenic.
Can children have bipolar disorder?
Yes. Children and adolescents can be diagnosed with bipolar disorder, though symptoms may look different than in adults.
In younger individuals, signs may include:
-
Rapid mood changes
-
Severe irritability
-
Behavioral outbursts
-
Changes in sleep and energy
The American Academy of Child and Adolescent Psychiatry (AACAP) emphasizes careful evaluation, as symptoms can overlap with ADHD or disruptive mood dysregulation disorder (DMDD).
What triggers bipolar episodes?
Common bipolar episode triggers include:
-
Sleep disruption
-
High stress or trauma
-
Substance use, including alcohol or stimulants
-
Medication changes or non-adherence
-
Seasonal changes (especially reduced daylight)
Managing triggers is a key component of relapse prevention, according to clinical guidance from NIMH.
How does bipolar disorder differ from borderline personality disorder?
Although often confused, bipolar disorder and borderline personality disorder (BPD) are distinct diagnoses.
Bipolar Disorder
-
Mood episodes last days to weeks
-
Episodes may occur without external triggers
-
Classified as a mood disorder
-
Strong biological and genetic basis
Borderline Personality Disorder
-
Mood shifts can occur within hours
-
Often triggered by interpersonal stress
-
Classified as a personality disorder
-
Core issues involve identity, abandonment fears, and emotional regulation
The DSM-5 clearly distinguishes these conditions, though some individuals may have co-occurring diagnoses.