Why Xylazine Is an Urgent Public Health Threat
Xylazine, known on the street as “tranq” or “tranq dope,” is a powerful veterinary sedative that has become one of the most alarming additions to the drug supply in recent years. Since around 2019–2020, this central nervous system depressant has been increasingly mixed with illicitly manufactured fentanyl and heroin, driving a surge in polysubstance overdoses and severe, life‑threatening wounds that have led some to call it the “zombie drug.”
Here’s what you need to know right now:
- Not approved for human use: Xylazine is FDA‑approved only for veterinary medicine and has never been approved for people anywhere in the world
- Often mixed with opioids: It is frequently found in mixtures with illicitly manufactured fentanyl and heroin, often without the user’s knowledge
- Not reversed by naloxone: Naloxone remains essential and can reverse the opioid portion of an overdose, but it does not counteract xylazine’s sedative or cardiovascular effects
- Declared an “emerging threat”: In April 2023, the White House Office of National Drug Control Policy (ONDCP) designated fentanyl adulterated or associated with xylazine (FAAX) as an “emerging drug threat” and released a National Response Plan in July 2023
- Now widely detected in deaths: In CDC-supported surveillance, xylazine was detected in up to about 11% of illicitly manufactured fentanyl–involved overdose deaths by mid‑2022, and in some Northeastern states in more than one quarter of such deaths
- Causes signature harms: People exposed to xylazine can develop deep necrotic skin ulcers, severe infections, and limb‑threatening wounds, along with dangerously low blood pressure and slowed breathing
What Is Xylazine?
Xylazine is an α2-adrenergic receptor agonist first synthesized by Bayer in 1962. Originally developed as a sedative, pain reliever, and muscle relaxant, it was intended for use in large animals such as horses, cattle, and deer. In veterinary medicine, it remains a valuable tool for procedural sedation, often combined with ketamine for surgeries and diagnostic procedures.
Early researchers explored xylazine for human use, including as a potential antihypertensive medication. However, human trials were discontinued after participants experienced severe adverse effects, including profound hypotension (dangerously low blood pressure) and significant central nervous system depression. These serious safety concerns meant xylazine was never approved for people.
Today, xylazine is FDA approved exclusively as a veterinary medicine in the United States. It has not been approved for human use anywhere in the world. Until recently, it was not classified as a controlled substance at the federal level, though many states began scheduling it in 2023 as a Schedule III substance in response to its growing presence in the illicit drug market.
Common legitimate veterinary uses include:
- Sedation and anesthesia, often combined with ketamine for surgical procedures
- Pre-anesthetic preparation for diagnostic imaging and minor procedures
- Occasionally as an emetic (to induce vomiting) in cats
On the street, xylazine is known as “tranq” or “tranq dope” when mixed with opioids—names that reflect its powerful sedative properties and its increasingly common presence in the drug supply that people who use drugs encounter daily.
Xylazine in the Illegal Drug Supply
Xylazine first appeared in the illicit drug supply in Puerto Rico’s heroin market during the early 2000s. From there, it spread to the mainland United States, where it has become increasingly common in fentanyl mixtures, heroin, and other substances sold on the street. Today, unwitting exposure to xylazine has become a significant concern for anyone using illicit drugs.
Why do dealers add xylazine? Several factors drive its proliferation:
- To intensify or prolong the effects of synthetic opioids like fentanyl
- To increase the bulk and weight of fentanyl powder or counterfeit fentanyl pills
- Because it’s cheap, potent, and was historically under-regulated compared to controlled substances
The numbers tell a stark story. According to the Drug Enforcement Administration, by 2022:
- Xylazine and fentanyl mixtures had been seized in 48 states
- Approximately 23% of fentanyl powder samples tested positive for xylazine
- About 7% of fentanyl pills seized contained xylazine
The DEA laboratory system continues to detect xylazine in a growing number of samples, and DEA reports widespread threat assessments have classified it among the deadliest drug threat concerns facing communities nationwide.
Xylazine is now found in:
- Fentanyl powder and pressed counterfeit pills (often sold as prescription medications like oxycodone)
- Heroin, cocaine, and methamphetamine in street markets
- Other drugs where users may have no idea xylazine is present
One critical challenge: most routine toxicology screens in emergency departments still do not test for xylazine detection. This means xylazine exposure is likely significantly under-recognized in overdose and poisoning cases across the country.
Health Effects and Overdose Risks
Understanding what xylazine does to the body is essential for protecting yourself and recognizing when someone needs help. As a potent central nervous system depressant, xylazine affects multiple body systems—and its dangers multiply dramatically when combined with opioids like fentanyl.
Acute Effects on the Body
When someone is exposed to xylazine, they may experience:
- Profound sedation, disorientation, and extreme drowsiness
- Slow breathing (respiratory depression) that can become life threatening
- Bradycardia (slow heart rate) and hypotension (low blood pressure)
- Reduced body temperature and severely impaired coordination
- Blurred vision and difficulty speaking or walking
Chronic Harms From Repeated Use
People with ongoing xylazine use often develop distinctive and devastating complications:
| Complication | Description |
|---|---|
| Xylazine associated wounds | Deep necrotic skin ulcers, abscesses, and cellulitis that can appear at injection sites or elsewhere on the body |
| Severe infections | Increased risk of sepsis, bone infections, and limb-threatening conditions |
| Amputation risk | Tissue death and severe wounds that may require surgical amputation |
| Skin infections | Poor wound healing that progresses despite basic first aid |
These characteristic skin wounds have contributed to xylazine’s “zombie drug” nickname—the tissue damage can be extensive and terrifying, leaving lasting scars even after healing.
Xylazine Overdose: A Complex Emergency
When xylazine is combined with fentanyl or other opioids, the risk of fatal overdose increases substantially:
- Prolonged unconsciousness and coma become more likely
- Both substances suppress breathing and heart function, compounding the danger
- Recovery time is extended because the sedative effects of xylazine persist even after naloxone is administered
🚨 Critical Note:
Naloxone reverses the opioid component of an opioid overdose but does not reverse xylazine’s effects on blood pressure, heart rate, or sedation. This means someone experiencing an overdose involving xylazine may remain unconscious and in danger even after receiving naloxone.
Xylazine Withdrawal
For people with chronic xylazine exposure, stopping use can trigger severe xylazine withdrawal symptoms that differ from—and add complexity to—standard opioid withdrawal. Symptoms may include intense anxiety, agitation, elevated heart rate, and profound discomfort. This creates additional challenges for addiction medicine specialists working to help people achieve recovery, as standard protocols for drug and alcohol dependence may need adaptation.
How to Reduce Harms for People Using Drugs Containing Xylazine
Many people do not know their drugs contain xylazine until they experience its effects—or worse, its complications. If you or someone you care about uses drugs that may be contaminated, practical harm reduction strategies can help reduce risks while you work toward your recovery goals.
Drug Checking and Awareness
- Use drug checking tools where available: Xylazine test strips and fentanyl test strips can help identify what’s in your supply. Some harm reduction organizations and syringe services programs offer rapid analysis through spectrometry services
- Recognize the signs: If drugs cause unusually prolonged sedation or if you notice skin changes after use, xylazine may be present
Never Use Alone
- Use with someone who can call 911 if you become unresponsive
- Consider overdose-prevention hotlines or digital check-in tools where available
- If alone, let someone know when and where you’re using
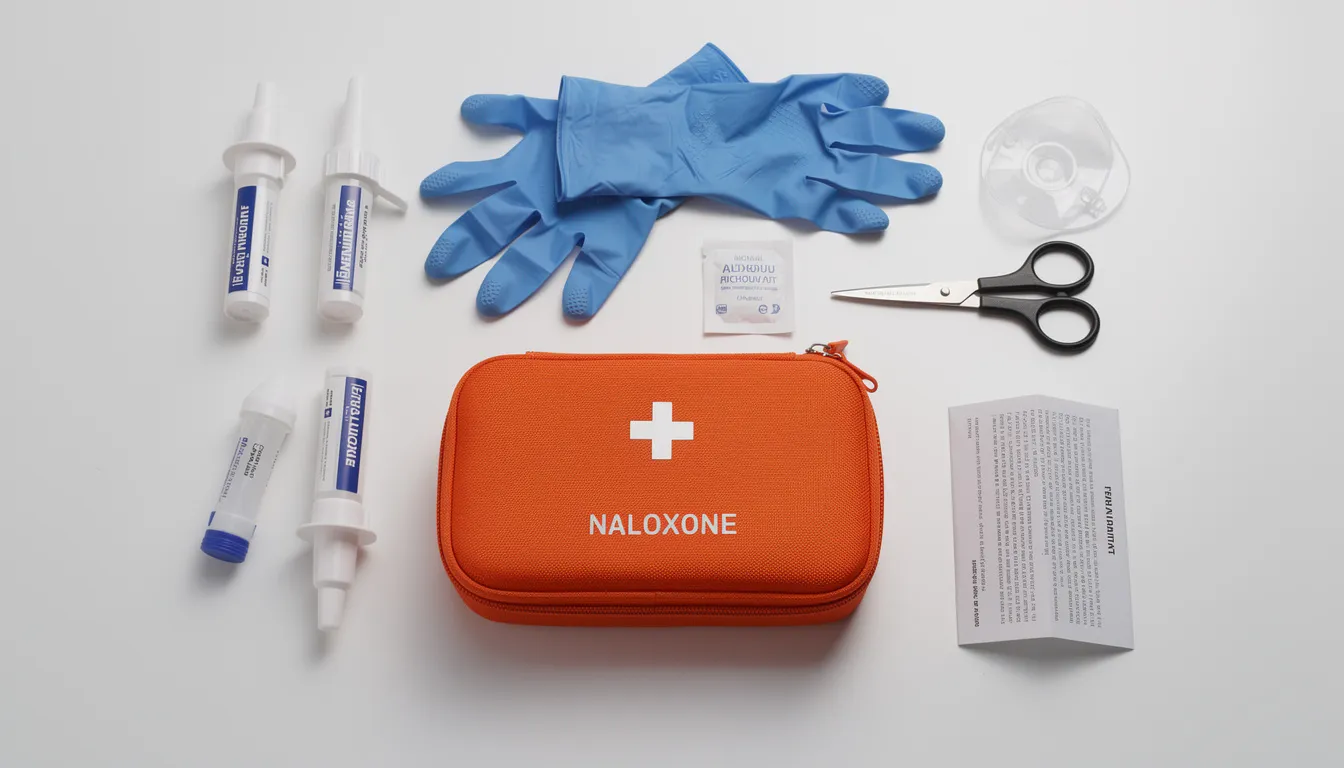
Always Carry Naloxone
Even though naloxone doesn’t reverse xylazine, it can still save a life by addressing the opioid part of a mixed overdose. Administer naloxone immediately if someone shows signs of overdose, then:
- Call 911
- Support breathing with rescue breaths if they’re not breathing adequately
- Stay with the person—xylazine’s effects may cause prolonged unconsciousness
Wound Care Is Essential
Xylazine related overdoses aren’t the only danger. Those characteristic severe wounds require attention:
- Monitor your body for new ulcers, skin changes, or areas of unusual pain
- Use sterile supplies and rotate injection sites if you inject
- Seek medical care early for any signs of infection: fever, spreading redness, foul odor, drainage, or blackening tissue
- Connect with needle exchange programs or wound care clinics—many syringe services programs now offer wound care services specifically for drug users
Connect With Treatment Resources
- Medications for opioid use disorder (MOUD) like buprenorphine and methadone can help stabilize recovery
- Low-barrier clinics and telehealth options have expanded since COVID-19 policy changes
- Urban health centers and harm reduction organizations often provide access without judgment
Remember: harm reduction strategies focus on making choices “safer,” not claiming any drug use is completely safe. Meeting people where they are is the first step toward lasting recovery.
Community and Healthcare Responses to the Xylazine Epidemic
Addressing the xylazine crisis requires coordination across multiple systems—public health agencies, law enforcement, emergency services, and social support networks. No single approach can solve this challenge, but together, communities are developing responses that save lives.
Public Health and Community Actions
Local and state health departments are taking important steps:
- Improving surveillance by adding xylazine to overdose toxicology testing and expanding drug-checking programs at harm reduction sites
- Launching education campaigns targeting people who use drugs, families, and first responders with clear messaging about xylazine risks
- Expanding harm reduction services including syringe services programs, naloxone distribution, safer-use supplies, and mobile outreach
Real-world example: Maryland’s syringe services programs detected xylazine in nearly 80% of opioid-containing samples during 2021-2022, prompting expanded education and resources. Colorado, while reporting fewer deaths, has established early monitoring systems and distributed harm reduct grants specifically for xylazine test strips.
What Health Care Professionals Should Do
For clinicians and first responders, several key practices can improve outcomes:
Consider xylazine exposure when a hospitalized patient shows opioid-like overdose symptoms but responds incompletely to naloxone, or when someone presents with unusual necrotic skin wounds
Provide supportive care for xylazine overdose, including:
- Airway management and supplemental oxygen
- IV fluids and blood pressure support
- Cardiac monitoring for slow heart rate and arrhythmias
Connect patients with ongoing care after stabilization:
- Addiction treatment and medications for opioid use disorder
- Harm reduction resources
- Specialized wound care services
Note for clinicians: The FDA has issued public safety alert communications urging awareness that routine urine drug screens do not detect xylazine. Specialized toxicology tests are recommended when xylazine is suspected. The National Institute on Drug Abuse and CDC Morbidity and Mortality Weekly Report publications have emphasized improved xylazine detection as a national drug control policy priority.
Data and Trends on Xylazine-Related Overdoses
The role of xylazine in overdose deaths has grown sharply over the past several years, particularly when combined with illicitly manufactured fentanyl. While systematic review of all jurisdictions remains incomplete, the available data paints a concerning picture.
National Trends
- Xylazine detection in drug samples increased substantially from 2020 to 2021, with the steepest growth in the Southern United States
- In monitored jurisdictions, the percentage of illicitly manufactured fentanyl–involved deaths with xylazine detected increased from about 2.9% in January 2019 to about 10.9% in June 2022
- Xylazine was detected in less than 12% of fentanyl‑involved deaths overall in these analyses, but levels varied widely by state and region
- In analyses of 10 U.S. cities, xylazine was involved in under 1% of overdose deaths in 2015 but had risen to nearly 7% by 2020
- CDC data shows xylazine in fentanyl-involved deaths rising from approximately 3% in January 2019 to around 11% by June 2022
Why the Numbers Are Likely Higher
The true scope of xylazine’s impact is almost certainly underestimated because:
- Many coroners and medical examiners still do not routinely test for xylazine
- Testing capacity varies widely between jurisdictions
- Cases from earlier years may not have tested positive simply because no one looked
Regional Patterns
| Region | Trend |
|---|---|
| Northeast | Earliest and highest concentration, especially Philadelphia and surrounding areas |
| Midwest | Significant spread by early 2020s |
| South | Steepest growth rates in recent years |
| West | Increasing detections, with states like Colorado implementing early monitoring |
Philadelphia’s data offers particularly stark evidence: in 2023, xylazine was involved in 38% of all unintentional overdose deaths in the city. Remarkably, 100% of xylazine-involved deaths also involved fentanyl or fentanyl analogues—confirming that xylazine rarely causes death alone but dramatically compounds the risks of the existing opioid crisis.
These xylazine-related overdoses represent a new layer of complexity in an already devastating epidemic. As testing expands and awareness grows, communities will gain a clearer picture of xylazine’s true toll.
Moving Forward: Hope in the Face of Challenge
The emergence of xylazine in the drug supply represents yet another obstacle in an already difficult landscape—but it’s one we can face together. Understanding what xylazine is, recognizing its signs, and knowing how to respond can genuinely save lives.
If you or someone you love is struggling with drug abuse or drug alcohol depend issues involving xylazine, fentanyl, or other substances, please know that recovery is possible. Treatment approaches are evolving to address the complexities of today’s drug supply, and compassionate care is available.
What you can do today:
- Learn to recognize xylazine’s effects and share this knowledge with others
- Ensure naloxone is accessible and everyone knows how to use it
- Seek wound care early if you notice any concerning skin changes
- Connect with treatment providers who understand the realities of xylazine and fentanyl
Your journey toward healing matters. The challenges posed by xylazine are real, but so is the possibility of a new beginning. If you’re ready to take the next step, reach out to a treatment center that understands what you’re facing—because no one should have to navigate this crisis alone.
Table of Contents
Check Your Coverage Now
"*" indicates required fields
Your information is kept private
Ready to Get Help?
Give us a call or fill out a contact form and we’ll reach out to you.


 By:
By:
 Editor:
Editor:
 Clinical Reviewer:
Clinical Reviewer: