
Does Narcan Work on Fentanyl? (Effectiveness, Limits, and What To Do in an Emergency)
Short Answer: Does Narcan Work on Fentanyl?
Yes, Narcan (naloxone) does work on fentanyl.
This medication functions as an opioid antagonist that rapidly reverses the life-threatening effects of opioid overdose, including those caused by fentanyl and its analogs. When someone stops breathing due to fentanyl exposure, naloxone can restore normal breathing within one to three minutes by displacing the opioid from receptors in the brain.
Because fentanyl and related synthetic opioids are exceptionally potent—at least 50 times stronger than heroin—multiple Narcan doses may be necessary to fully reverse an overdose. However, this does not mean the medication fails. It means the clinical approach requires repeated dosing, a protocol that emergency responders and harm reduction programs use successfully every day.
As of late summer 2023, Narcan nasal spray (4 mg naloxone HCl per spray) became available over the counter throughout the United States. This expanded access reflects the medical community’s confidence in naloxone’s safety and effectiveness. It’s important to understand that while Narcan will not reverse overdoses from non-opioid substances like methamphetamine, cocaine alone, benzodiazepines, or xylazine, it should still be administered whenever an opioid overdose is suspected. The medication causes no harm if given to someone who hasn’t taken opioids.
Key Takeaways:
- Narcan is effective against fentanyl and remains the recommended first-line response for suspected opioid overdose
- Multiple doses may be required due to fentanyl’s extreme potency, but this is expected and does not indicate failure
- Narcan is now available without a prescription at pharmacies nationwide, making it accessible to anyone who might witness an overdose
What Is Fentanyl and Why Is It So Dangerous?
Fentanyl is a synthetic opioid that represents one of the most significant challenges in the current overdose crisis. Originally developed for managing severe pain in medical settings, this substance is approximately 50 to 100 times more potent than morphine and at least 50 times stronger than heroin. This extraordinary potency means that quantities invisible to the naked eye can cause a fatal overdose, particularly in individuals without opioid tolerance.
Understanding the distinction between prescription fentanyl and illicitly manufactured fentanyl is essential. Medically prescribed fentanyl comes in carefully controlled formulations—transdermal patches, lozenges, or intravenous solutions administered during surgery or for cancer pain treatment. These are dispensed by a doctor and used under medical supervision. Illicitly manufactured fentanyl, however, enters the drug supply through clandestine laboratories and appears as powders, fake prescription pills, or adulterants mixed into cocaine, heroin, or methamphetamine.
The Centers for Disease Control and Prevention (CDC) estimates that in 2022, approximately 83,000 U.S. overdose deaths involved opioids, with fentanyl and other powerful synthetic opioids driving the sharp increase. This reality affects communities across the country, including adolescents and children who may unknowingly encounter fentanyl in counterfeit pills purchased through social media or from peers.
Key Facts About Fentanyl:
- Extreme potency: A dose as small as a few grains resembling table salt can be lethal, especially for people with no opioid tolerance
- Fake pills are common: Counterfeit versions of oxycodone, Percocet, Xanax, and other prescription pills often contain unpredictable, dangerous amounts of fentanyl
- Widespread contamination: Illegal opioids, cocaine, methamphetamine, and illicit drugs may contain fentanyl mixed without the user’s knowledge
- Higher risk populations: Adolescents, children, and anyone without opioid tolerance face elevated danger from even minimal exposure
- Unpredictable distribution: Fentanyl may be unevenly distributed in pills or powders, meaning one pill could be safe while another from the same batch is lethal
How Narcan (Naloxone) Works Against Fentanyl
Naloxone functions as a pure opioid receptor antagonist with the highest affinity for the mu-opioid receptor in the central nervous system. In practical terms, this means it competes directly with opioids like fentanyl for receptor binding sites in the brain. When administered during an overdose, naloxone rapidly displaces fentanyl from these receptors, effectively “kicking out” the drug and restoring normal respiratory function.
The mechanism works identically regardless of which opioid caused the overdose. Whether the substance involved is fentanyl, heroin, oxycodone, hydrocodone, morphine, or methadone, naloxone blocks the opioid’s effects at the receptor level. This is why addiction medicine specialists and emergency responders rely on it as the universal antidote for opioid toxicity.
Why Fentanyl May Require Multiple Doses:
- High potency and tight receptor binding: Fentanyl binds strongly to opioid receptors, sometimes requiring more naloxone to fully displace it
- Large doses or repeated exposure: Someone who has used significant amounts may need additional naloxone to overcome the opioid load
- Co-use with other depressants: When fentanyl is combined with alcohol, benzodiazepines, or xylazine, the sedation from non-opioid substances won’t respond to naloxone, potentially masking improvement
Research and real-world experience from emergency medical services and harm reduction programs consistently demonstrate that naloxone remains effective for fentanyl overdoses. The need for repeated dosing is a recognized clinical protocol, not a limitation of the medicine itself.
Myth vs. Fact:
- Myth: “Narcan doesn’t work on fentanyl because it’s too strong”
- Fact: Naloxone works through the same mechanism on fentanyl as on any opioid. When outcomes are poor, the issue is typically delayed administration, insufficient doses, or the presence of non-opioid substances—not naloxone failure
Recognizing a Fentanyl or Other Opioid Overdose
The signs of fentanyl overdose mirror those of other opioid overdoses but may progress more rapidly due to the substance’s potency. Recognizing these signs quickly is critical because every minute without oxygen increases the risk of brain damage or death.
Classic Opioid Overdose Symptoms:
| Category | Signs to Watch For |
|---|---|
| Consciousness | Unresponsive to shouting, shaking, or painful stimulation (knuckle rub on breastbone) |
| Breathing | Slow, shallow, or stopped breathing; snoring, gurgling, or choking sounds |
| Skin appearance | Pale, cold, clammy, or gray/blue coloring, especially around lips and fingertips |
| Physical state | Limp body, slow or absent pulse |
| Eyes | Pinpoint pupils (very small black centers) |
Assume fentanyl could be involved if:
- You see powders, pills, foil, or syringes nearby
- The person used drugs sold as heroin, oxycodone, Xanax, cocaine, or “blues”
- They took a pill purchased on social media, from a friend, or from any unregulated source
- Any fake pills or substances of unknown origin were involved
Act immediately. Do not wait to be certain which drug was used. Narcan is safe to administer even if you’re wrong about the substance involved—it will not cause harm to someone who hasn’t taken opioids.
Step-by-Step: How to Use Narcan in a Suspected Fentanyl Overdose
These instructions apply to any suspected opioid overdose, including those potentially involving fentanyl. Acting quickly and systematically gives the person the best chance of survival.
Step 1: Check for Responsiveness Shake the person firmly and shout their name. If there’s no response, try rubbing your knuckles hard on their breastbone (sternum rub). If they don’t wake up or respond, treat this as an emergency.
Step 2: Call 911 Immediately Contact emergency services and clearly state “suspected opioid overdose” or “suspected fentanyl overdose.” Stay on the line if possible—dispatchers can provide guidance while you help.
Step 3: Administer Narcan Nasal Spray Tilt the person’s head back slightly. Insert the nozzle of the nasal spray into one nostril until your fingers touch the bottom of their nose. Press the plunger firmly to deliver the full dose. Each spray is a complete dose.
Step 4: Provide Rescue Breathing If you’re trained and the person isn’t breathing (or breathing is very slow), give rescue breaths. Tilt their head back, lift their chin, pinch their nose closed, and give one breath every five seconds.
Step 5: Give a Second Dose If Needed If there’s no response within 2-3 minutes—no change in breathing, no movement—give a second Narcan dose in the other nostril.
Step 6: Continue Dosing Until Help Arrives If you have additional Narcan and the person still isn’t breathing or waking up, continue giving doses every 2-3 minutes. Fentanyl overdoses commonly require multiple doses.
After the Person Responds:
- Place them in the recovery position (on their side with their top knee bent forward) to prevent choking if they vomit
- Stay with them until emergency responders arrive
- Monitor for signs of the overdose returning, as naloxone may wear off before the fentanyl does
Expected Withdrawal Symptoms After Narcan: When naloxone reverses an overdose in someone with opioid dependence, they may experience opioid withdrawal symptoms including agitation, nausea, vomiting, body aches, sweating, anxiety, and diarrhea. These symptoms are uncomfortable but far less dangerous than the alternative of not reversing the overdose.
Does Narcan Always Work on Fentanyl? (Limits and Challenges)
Narcan is highly effective, but outcomes depend on several factors that influence whether the reversal is complete and sustained. Understanding these variables helps set realistic expectations while reinforcing the importance of rapid response.
Factors Affecting Narcan Effectiveness:
| Factor | Impact on Outcome |
|---|---|
| Amount of fentanyl consumed | Higher doses or more potent analogs (like carfentanil) require more naloxone |
| Time to administration | The faster Narcan is given after breathing slows, the better the outcome |
| Presence of other drugs | Sedatives like benzodiazepines, alcohol, or xylazine won’t respond to naloxone |
| Underlying health conditions | Pre-existing lung or heart disease may complicate recovery |
When “Narcan Didn’t Work” Actually Means:
- Administration came too late, after prolonged oxygen deprivation had already caused damage
- Insufficient doses were given for the amount of opioid present
- The primary substance wasn’t an opioid (test strips later confirm no fentanyl, or xylazine alone was involved)
The Rebound Risk
Because naloxone has a shorter half-life (30-90 minutes) than many opioids, including fentanyl, methadone, and extended-release formulations, the overdose can return after naloxone wears off. This is why calling 911 and seeking emergency department care are non-negotiable, even if the person wakes up and seems fine. Medical professionals may use IV naloxone infusions or repeated dosing to manage severe cases—evidence that the medication works, but sometimes needs sustained administration.
Narcan vs. Non-Opioid Additives: Xylazine and Other Emerging Threats
Xylazine, a veterinary sedative often called “tranq,” has emerged as a significant concern in the drug supply. First detected at high levels in the Northeast around 2019-2020, xylazine is now found mixed with fentanyl and heroin across the country. Understanding its interaction with naloxone is crucial for anyone who might respond to an overdose.
Key Facts About Xylazine:
- It is not an opioid and therefore does not respond to Narcan
- It causes profound sedation, slowed breathing, and dangerously low blood pressure
- It can cause severe skin wounds at injection sites
When Fentanyl and Xylazine Are Both Present:
- Narcan can reverse the fentanyl component and may partially improve breathing
- Sedation may persist because xylazine effects remain unblocked
- The person may not wake up fully even after appropriate naloxone dosing
- Emergency medical care is essential for oxygen support, airway management, and monitoring
Other Emerging Synthetic Opioids: Substances like nitazenes and various fentanyl analogs represent newer threats in the illicit drug supply. Most of these synthetic opioids remain responsive to naloxone, though they may require higher or repeated doses due to their potency.
Bottom Line: In any suspected overdose, give someone naloxone first. It may help, it won’t hurt, and you cannot determine what other drugs are present in the moment. But never view Narcan as a substitute for emergency medical care.
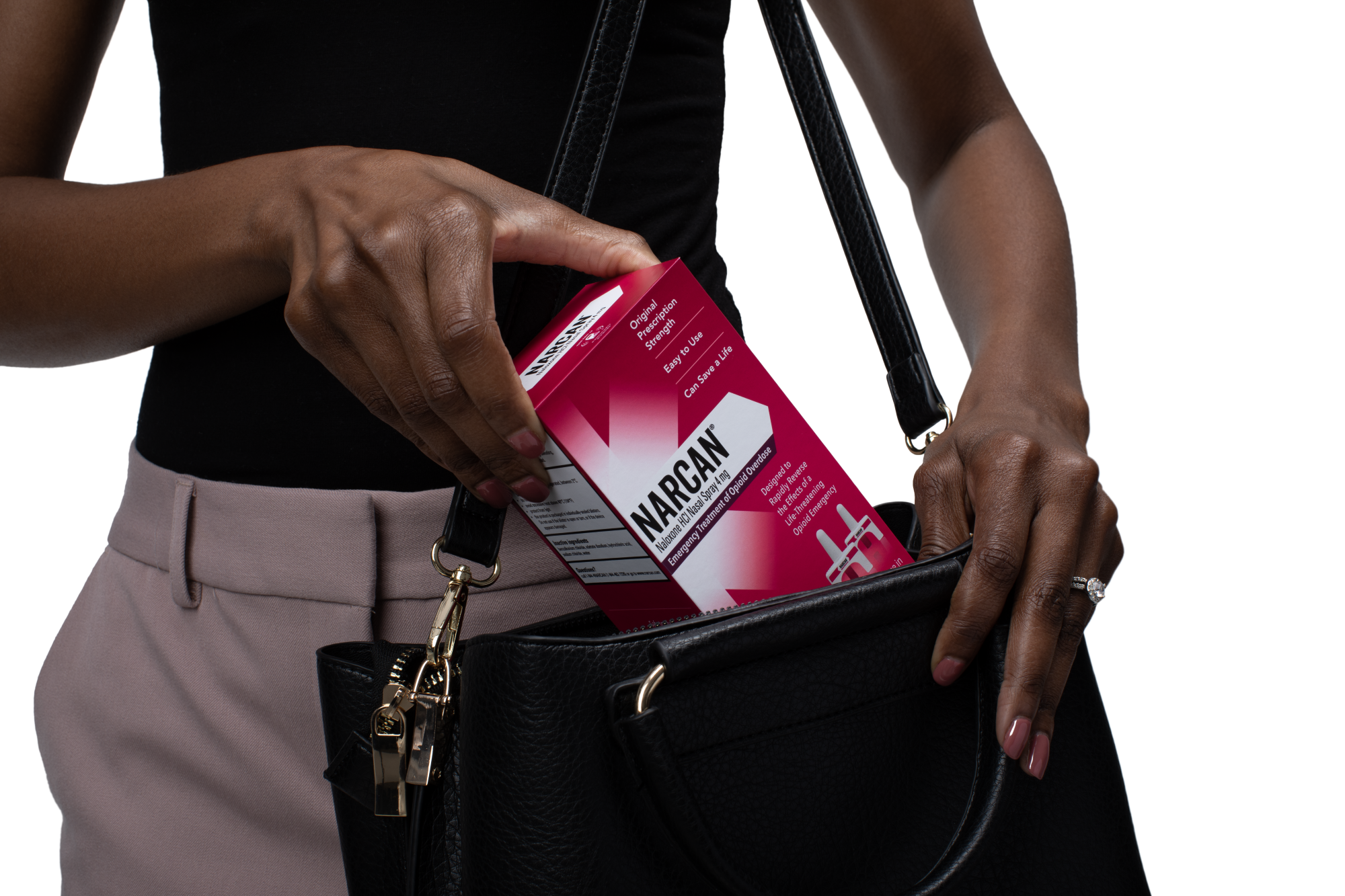
Who Should Carry Narcan in the Fentanyl Era?
The widespread presence of fentanyl in the drug supply means that overdose risk extends far beyond what many people expect. Anyone who might witness an opioid overdose should consider keeping Narcan accessible.
Groups Who Should Carry Naloxone:
- People who use opioids (heroin, fentanyl, prescription pain pills) whether prescribed or not
- People who use non-opioid street drugs (cocaine, methamphetamine, MDMA) that may be contaminated with fentanyl
- Friends, partners, and family members of people who use drugs
- Households with prescription opioids where children or teens might access medication
- Staff at bars, clubs, homeless shelters, schools, universities, and community organizations
- First responders, security personnel, and anyone working with the public
Think of Narcan the same way you’d think of an EpiPen for severe allergies or a fire extinguisher in your kitchen. It’s simple safety equipment designed for emergencies you hope never happen but need to be prepared for.
Critical Reminder: Someone experiencing an overdose cannot administer Narcan to themselves. Make sure people around you know where your Narcan is kept and how to use it.
Where and How to Get Narcan If You’re Worried About Fentanyl
Access to naloxone has never been easier. Following FDA approval for over-the-counter sales in late 2023, Narcan nasal spray is available without a prescription throughout the United States.
Where to Find Narcan:
| Source | Details |
|---|---|
| Chain and independent pharmacies | Available over the counter; no prescription needed for OTC brands |
| Grocery stores and big-box retailers | Many now stock Narcan in the pharmacy or first aid section |
| Drug stores | Most major chains carry OTC naloxone products |
| Online retailers | OTC Narcan available for shipping nationwide |
| Local pharmacy with standing orders | Some prescription formulations available through state protocols |
| Community harm reduction programs | Often available for free |
| Syringe services programs | Typically distribute naloxone alongside other supplies |
| Local health departments | Many offer free naloxone through disease control and prevention initiatives |
| College and university health centers | Increasingly common on campuses |
Insurance and Cost Considerations:
- Private insurance, Medicaid, and Medicare often cover prescription naloxone with low or no copay
- Manufacturer patient assistance programs and discount cards may reduce out-of-pocket costs
- Many community programs distribute naloxone for free regardless of insurance status
For Readers Outside the U.S.: Naloxone availability and regulations vary by country and region. Check with your local health authority or pharmacy to understand access in your area.
Fentanyl Test Strips and Other Harm Reduction Tools Alongside Narcan
Fentanyl test strips are small strips that detect the presence of fentanyl in pills, powders, and some liquids before use. They function similarly to home pregnancy tests—you dissolve a small amount of the substance in water, dip the strip, and read the results.
How Test Strips Work:
- Add a small amount of the drug to water
- Dip the strip for the specified time
- Read results (one line typically indicates fentanyl presence; two lines indicate no fentanyl detected)
- Results appear within minutes
Important Limitations:
- Test strips may not detect all fentanyl analogs
- Fentanyl distributed unevenly in a pill means testing one portion doesn’t guarantee the rest is safe
- A negative result doesn’t mean the substance is safe—other dangerous drugs may be present
Legal Considerations: Many states have reclassified fentanyl test strips as public health tools rather than drug paraphernalia, but laws still vary. Check your local regulations.
Combining Harm Reduction Strategies:
- Use test strips to identify potential fentanyl presence
- Carry naloxone for emergencies
- Never use alone; have someone present who can call 911 and administer Narcan
- Access sterile supplies through local harm reduction programs
- Connect with treatment resources for opioid use disorder when ready
Many overdose prevention kits now include both Narcan and fentanyl test strips, along with brief training that takes less than 10 minutes to complete. These tools work together to save lives.
Safety of Narcan for Children, Teens, and Adults
Naloxone has been safely used by medical professionals for over 40 years. In all that time, no overdose deaths have been attributed to naloxone itself. The medication is considered safe across all age groups—infants, children, adolescents, adults, and older adults—when opioid overdose is suspected.
There Is No Downside to Giving Narcan:
- It will not get anyone “high”
- It cannot cause an overdose
- It will not harm someone who hasn’t taken opioids
- If the cause of collapse turns out to be something else (seizure, heart attack, diabetic emergency), naloxone simply won’t have an effect
Withdrawal After Narcan: When naloxone reverses an overdose in someone with physical dependence on opioids, withdrawal symptoms may occur. In infants, this might appear as crying and irritability. In adolescents and adults, expect potential agitation, nausea, vomiting, sweating, body aches, and anxiety. These symptoms are uncomfortable—sometimes intensely so—but they are not life-threatening. The alternative of not reversing the overdose is far more dangerous.
Special Considerations: Newborns being treated in medical settings for neonatal opioid withdrawal syndrome receive care under specialized pediatric protocols. This is a clinical situation managed by medical professionals, not something bystanders should attempt at home.
The principle is simple: when in doubt, give Narcan. Better safe than sorry.
Legal Protections and Why You Should Still Call 911
Most U.S. states have enacted Good Samaritan or overdose immunity laws that provide some legal protection for people who call 911 in good faith during an overdose emergency. These protections typically apply to:
- The person experiencing the overdose
- The person who calls for help
- Others present at the scene
What These Laws Generally Cover:
- Protection from prosecution for drug possession (amounts vary by state)
- Protection from certain parole or probation violations in some states
- Protection for administering naloxone in good faith
Important Caveats: Laws differ significantly by state. Some offer broader protections than others. However, fear of legal consequences should never stop you from calling for help. The priority is preserving life.
Why 911 Is Always Necessary:
- Narcan is temporary; its effects last 30-90 minutes
- Fentanyl and longer-acting opioids may outlast naloxone
- Breathing can slow again after the person initially wakes up
- Medical professionals can provide sustained monitoring, additional naloxone, and treatment for complications
When Speaking with Dispatch:
- State clearly that you have a suspected opioid or fentanyl overdose
- Mention that Narcan has been given and how many doses
- Provide your location and stay on the line for instructions
Stay with the person until emergency responders arrive. Do not leave them alone, even if they seem recovered.
Key Takeaways: Narcan and Fentanyl
- Narcan does work on fentanyl and is the critical first-line response to any suspected opioid overdose
- Multiple doses are often needed because fentanyl is extremely potent—this is expected, not a sign of failure
- Narcan is safe and available over the counter at your local pharmacy, making it accessible to most people who might witness an overdose
- Fentanyl test strips complement naloxone by helping identify risk before use, though they have limitations
- Never use alone whenever possible; having someone present who can call 911 and give Narcan dramatically improves survival odds
- Narcan is not a replacement for medical care—always call emergency services and stay with the person until help arrives
- Treatment for substance use and opioid use disorder is available and effective for those ready to explore recovery options
Understanding how naloxone works empowers you to act decisively when minutes matter. If you or someone you care about faces risks related to opioid use, having Narcan on hand is a straightforward step that can save lives. Contact your local pharmacy or harm reduction program to obtain naloxone, and consider reaching out to treatment professionals like those at Legacy Healing Center to explore comprehensive care options for lasting recovery.
Frequently Asked
Questions about Narcan
Can fentanyl be treated with Narcan?
Yes. Narcan (the brand name for naloxone) can reverse a fentanyl overdose.
Naloxone works by:
-
Rapidly binding to opioid receptors
-
Displacing fentanyl and other opioids
-
Reversing respiratory depression, the primary cause of opioid overdose deaths
The Centers for Disease Control and Prevention (CDC), National Institute on Drug Abuse (NIDA), and Substance Abuse and Mental Health Services Administration (SAMHSA) all confirm that naloxone is effective against synthetic opioids, including fentanyl.
Important note:
Because fentanyl is extremely potent, multiple doses of Narcan may be required, and emergency medical care is still essential.
What drug does Narcan not work on?
Narcan only works on opioids. It does not reverse overdoses caused by non-opioid substances, including:
-
Alcohol
-
Benzodiazepines (e.g., Xanax, Valium)
-
Stimulants (e.g., cocaine, methamphetamine)
-
Synthetic drugs that are not opioids
If Narcan is given during a non-opioid overdose, it will not cause harm, but it also will not reverse the overdose.
Because many overdoses involve multiple substances, the CDC recommends administering Narcan anytime an opioid overdose is suspected.
What is the antidote for fentanyl overdose?
The antidote for a fentanyl overdose is naloxone.
Naloxone is:
-
FDA-approved
-
Available as a nasal spray (Narcan, Kloxxado) or injectable
-
Safe and non-addictive
-
Effective within 2–3 minutes in most cases
Naloxone is recognized by the FDA, CDC, and World Health Organization (WHO) as an essential life-saving medication for opioid overdoses.
How long does Narcan block fentanyl?
Narcan typically works for 30 to 90 minutes, depending on:
-
Dose administered
-
Potency of the opioid
-
Route of exposure
Fentanyl often lasts longer in the body than naloxone, which means:
-
Overdose symptoms can return after Narcan wears off
-
Repeated doses may be needed
-
Emergency medical care is critical, even if the person wakes up
SAMHSA and emergency medicine guidelines emphasize that Narcan is a temporary reversal, not a substitute for hospital treatment.










