
What You Need to Know about Intensive Outpatient Programs (IOP)
-
 By:
Valerie Puffenberger, PMHNP-BC
By:
Valerie Puffenberger, PMHNP-BC
-
 Editor:
Phyllis Rodriguez, PMHNP-BC
Editor:
Phyllis Rodriguez, PMHNP-BC
-
 Clinical Reviewer:
Dr. Ash Bhatt, MD, MRO
Clinical Reviewer:
Dr. Ash Bhatt, MD, MRO
Introduction to Mental Health Treatment
Your mental health and healing journey is precious, and finding the right support can feel overwhelming when you’re navigating challenges like depression, anxiety, or substance use. If you’re looking for comprehensive care that honors your daily life — your work, your family, your home — intensive outpatient programs offer a beautiful bridge between getting the help you need and maintaining the connections that matter most to you. These programs understand that your recovery happens not just in treatment rooms, but in the real moments of your everyday life.
The Substance Abuse and Mental Health Services Administration recognizes these programs as essential stepping stones in your healing journey, and there’s a reason why. Through a compassionate blend of group connection, individual guidance, and practical life skills, you’ll find the support you need to not just manage what you’re facing, but to truly transform your relationship with your mental health and substance use. This isn’t about fitting you into a one-size-fits-all approach — it’s about meeting you exactly where you are and helping you build the resilience and tools for lasting change. Whether you’re taking your first brave step toward healing or continuing on your path of recovery, these programs offer hope-filled, personalized support designed to help you move from surviving to truly thriving in the life you deserve.
Intensive Outpatient – Fast Facts
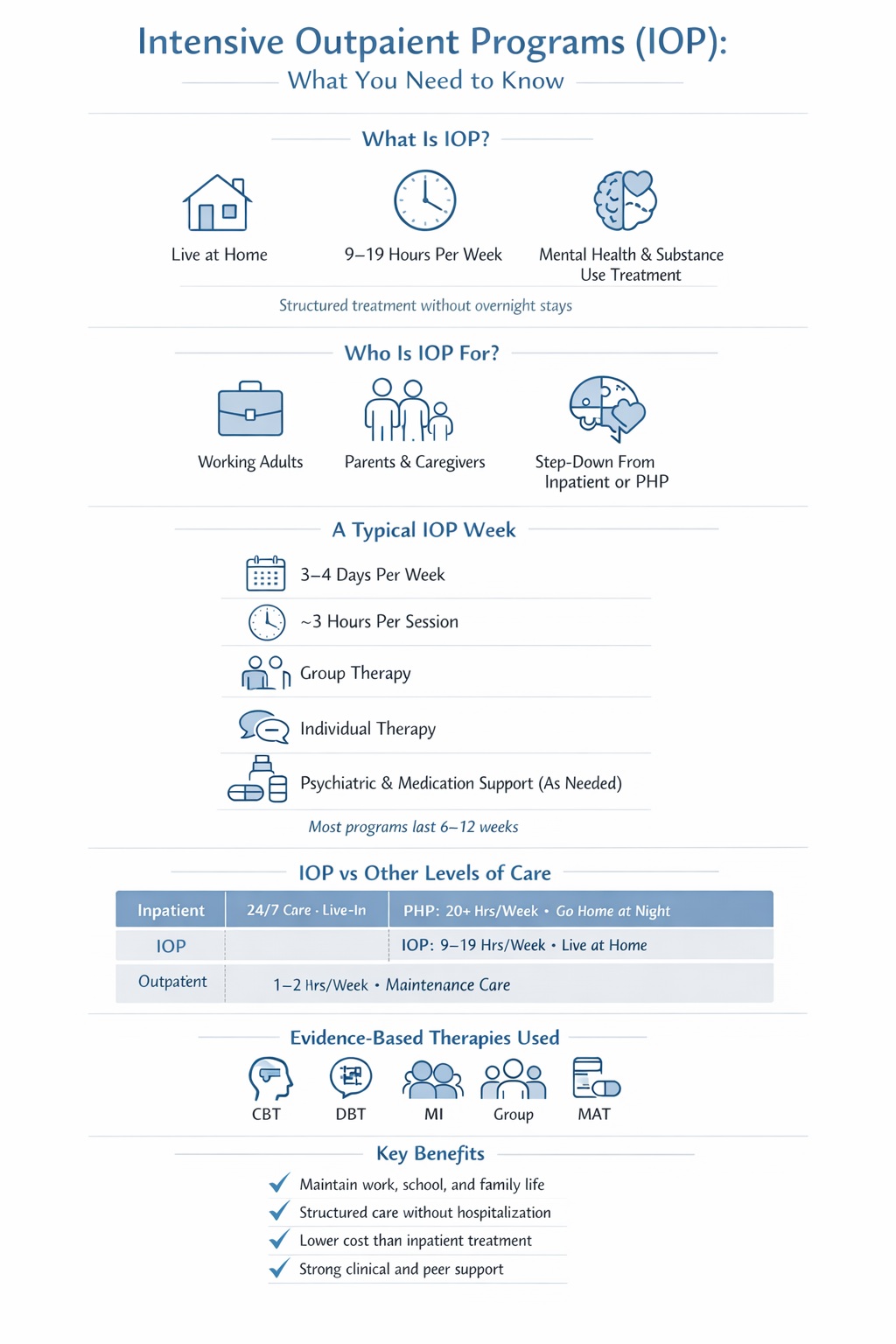
An intensive outpatient program provides structured, evidence-based treatment for mental health conditions and substance use disorders without requiring you to live at a treatment facility. It’s designed for people who need more than weekly therapy but don’t require 24-hour supervision—offering the support to sustain recovery while keeping daily life intact.
- 9–19 therapy hours per week spread across 3–4 days, typically 3 hours per session
- Keep working, attending school, or caring for family while receiving intensive treatment
- Evidence based treatments like cognitive behavioral therapy, motivational interviewing, and dialectical behavior therapy
- Typical program length of 8–12 weeks, with flexibility based on individual progress
- In-person and telehealth options available at most programs through 2025 schedules
- Widely covered by commercial insurance, Medicaid, and Medicare across the United States, but insurance may cover all or at least part of the cost—coverage varies by plan, so check with your provider for details.
IOPs generally cost less than inpatient programs since they do not provide 24/7 care or include room and board.
IOPs operate in hospital-based programs, community mental health centers, and private treatment networks nationwide. Whether you’re stepping down from residential care or stepping up from standard outpatient, this level of care meets you where you are.
What is an Intensive Outpatient Program?
An intensive outpatient program is a structured, time-limited treatment program that delivers 9–19 hours of psychiatric services and behavioral health support each week. Unlike inpatient treatment or residential programs, you don’t stay overnight—you attend scheduled sessions and return home to your normal environments between appointments.
IOPs sit between standard once-a-week outpatient therapy and higher levels of care like partial hospitalization (PHP) or residential treatment. The mental health services administration and addiction medicine communities recognize IOP as ASAM Level 2.1 care, positioning it as a meaningful step in the continuum of care that can prevent hospitalization or support a safe transition after discharge.
Typical clinical components include:
- Group therapy and group counseling sessions (the core of most programs)
- Individual therapy with a licensed clinician
- Family sessions and educational services for loved ones
- Psychiatric evaluation and ongoing medication management
- Skills training in areas like emotional regulation, coping strategies, and communication
- Psychoeducation about your specific condition and relapse triggers
Programs can be specialized for particular needs—mood disorders, trauma recovery, co-occurring substance abuse and depression, or specific tracks. Most operate Monday through Friday on fixed morning, afternoon, or evening schedules. Each program follows national guidelines endorsed by organizations like SAMHSA and uses evidence-based protocols to ensure you receive comprehensive care that works.
Who Benefits from Intensive Outpatient Treatment?
Intensive outpatient treatment works best for people who need more support than weekly therapy provides but don’t require around-the-clock supervision or medical detox. If you’re ready to attend treatment multiple times per week and can manage daily responsibilities between sessions, IOP may be the right fit.
Common situations where IOP helps:
- Stepping down after completing inpatient or PHP (such as after a 7–28 day residential stay)
- Stepping up from traditional outpatient because symptoms are worsening
- Returning to structured care after a relapse following a period of sobriety
- Managing acute stress reactions, grief, or trauma that disrupts daily functioning
- Stabilizing after a psychiatric crisis while maintaining work or school
- Addressing a specific substance use pattern that requires intensive treatment but not residential placement
Who attends IOP:
- Adults with depression, anxiety, bipolar disorder, or other mental health conditions needing stabilization
- People with alcohol, opioid, or other substance use disorders who are medically stable
- Teens struggling academically or socially due to behavioral health challenges
- Working professionals who need intensive treatment without taking extended leave
- Parents and caregivers who can’t step away from family responsibilities for weeks at a time
To be a good candidate, you must be safe enough to live in the community—no immediate risk of harm to yourself or others—and able to attend sessions reliably, whether through transportation or telehealth access. A licensed clinician such as a physician, psychiatrist, psychologist, or therapist should complete an assessment to confirm IOP is the appropriate level of care for your situation.
Lasting Results: Kevin regained self-respect and learned practical tools to stay grounded in recovery. He has new friends and a new lease on life.

Intensive Outpatient vs. Inpatient and Other Levels of Care
Understanding where IOP fits helps you make an informed decision. The continuum of care moves from most intensive (medical detox and inpatient) through mid-level options (PHP, IOP) down to standard outpatient and peer support. Each level serves different clinical needs.
- Inpatient and residential care provides 24-hour supervision with on-site housing. This level is appropriate when you need medically managed detox, constant monitoring, or a completely controlled environment. Stays typically range from 3–30 days for acute psychiatric admissions or substance abuse treatment.
- Partial hospitalization (PHP) delivers 20 or more hours of treatment per week—often 5 days, 4–6 hours daily. You go home at night, but daytime hours are largely occupied by treatment. PHP suits people transitioning from inpatient who still need substantial structure.
- Intensive outpatient provides 9–19 hours weekly, usually 3–4 days for about 3 hours per session. This is the level where you can maintain work, school, parenting, or caregiving while receiving effective treatment.
- Standard outpatient involves 1–2 hours weekly or less—typically individual therapy or medication management appointments. This works well for maintenance once symptoms stabilize and you’ve built solid coping skills.
| Level of Care | Setting | Hours per Week | Supervision | Typical Length |
|---|---|---|---|---|
| Inpatient/Residential | Live at facility | 24/7 | Continuous medical and psychiatric | 3–30 days |
| Partial Hospitalization (PHP) | Attend daily, go home at night | 20+ hours | Structured daytime programming | 2–4 weeks |
| Intensive Outpatient (IOP) | Attend sessions, live at home | 9–19 hours | Scheduled sessions only | 6–12 weeks |
| Standard Outpatient | Office visits | 1–2 hours | Appointment-based | Ongoing as needed |
Many people move through multiple levels as they progress. Starting with higher level care and stepping down to IOP is common—and so is stepping back up if symptoms worsen. The goal is always matching the right intensity to your current needs.
What to Expect in an Intensive Outpatient Program
Most IOPs follow a predictable weekly routine that combines group sessions, individual therapy, and medication or psychiatric visits. Knowing what’s ahead can ease the uncertainty of starting something new.
A typical week might include:
- 3 days of programming (Monday, Wednesday, Friday)
- 3-hour sessions each day (9:00 a.m.–12:00 p.m. or 6:00 p.m.–9:00 p.m.)
- One individual therapy session (weekly or biweekly)
- Occasional family sessions or psychiatric appointments scheduled separately
Intake and assessment happens before you begin the full program. During this process, you’ll complete a clinical assessment covering safety, diagnostic clarification, baseline symptom measures, and—for substance use programs—current use patterns. Together with your treatment team, you’ll develop a written treatment plan with concrete goals tailored to your situation.
Each week typically includes:
- Psychoeducation groups covering topics like depression, trauma, or cravings
- Process groups where you share experiences and receive peer feedback
- Skills training focused on coping strategies, communication, and problem-solving
- Medication review with prescribing clinicians as needed
- Recovery and aftercare planning that evolves throughout your stay
Programs require consistent attendance. If you’re in a substance use track, expect urine drug screens as a routine part of monitoring. Many programs assign homework—journaling, practicing skills, or completing worksheets—so you can apply what you learn between sessions in real-world situations.
Flexible Scheduling and Program Formats
Real-world programs understand that one schedule doesn’t fit everyone. That’s why flexibility is built into most IOPs:
- Morning tracks: 9:00 a.m.–12:00 p.m., ideal for those with afternoon or evening work shifts
- Afternoon tracks: 1:00 p.m.–4:00 p.m., suitable for morning obligations
- Evening tracks: 6:00 p.m.–9:00 p.m., designed for people working traditional daytime hours
- Weekend options: Some programs offer Saturday sessions for added flexibility
Hybrid and virtual IOPs deliver the same structured programming through secure telehealth platforms. These expanded significantly after 2020 and continue through 2025, making intensive treatment accessible regardless of transportation or geography.
Programs often run separate tracks for adults, adolescents, and sometimes working professionals. As you progress, attendance requirements may adjust—moving from 4 days weekly to 3, for example—based on your stability and clinical need.
Therapeutic Groups and Skills Training
Group therapy is the backbone of most IOPs. Group members meet multiple times weekly, creating a community of support that’s hard to replicate in individual sessions alone.
Types of group sessions you’ll encounter:
- Process groups focused on sharing experiences, receiving feedback, and practicing vulnerability in a safe space
- Psychoeducational groups teaching you about your diagnosis, the treatment process, and recovery principles
- CBT skills practice where you learn to identify personal patterns, challenge unhelpful thoughts, and develop skills to manage triggers and other challenges encountered during recovery. CBT also teaches clients skills to recognize and reduce relapse risks, maintain abstinence, and enhance self-efficacy.
- Relapse prevention groups focused on recognizing relapse triggers and building response plans
- Emotional regulation and communication groups teaching practical skills for daily life
Evidence-based group modalities often include:
- Cognitive behavioral therapy exercises
- Dialectical behavior therapy (DBT) skills modules
- Mindfulness-based relapse prevention techniques
- 12-Step discussion and integration groups
Practical topics you’ll work on:
- Identifying triggers and craving cues for your specific substance or symptom patterns
- Developing coping plans for high-risk situations like weekends and holidays
- Managing panic symptoms or depressive episodes when they arise
- Repairing relationships damaged by substance use or mental health struggles
- Building self efficacy through small, achievable goals
Individual Therapy, Psychiatric Services, and Medication Support
While groups form the core of IOP, individual sessions provide space for personalized work that doesn’t fit the group format.
- Individual therapy typically occurs weekly or biweekly with a licensed therapist to address trauma, identify personal treatment goals, manage crises, and work through sensitive issues
- Psychiatric evaluation happens at intake with a psychiatrist or psychiatric nurse practitioner who assesses medication needs
- Medication management includes follow-up visits to adjust antidepressants, mood stabilizers, anti-anxiety medications, or medications for addiction treatment like naltrexone or buprenorphine
- Coordination of care ensures your IOP team communicates with your primary care physician, existing therapist, or probation officer when relevant
For those in substance use programs, medication-assisted treatment (MAT) can be integrated directly into your IOP treatment alongside counseling and behavioral therapies. This combination—medication plus therapy—often produces the best treatment outcomes for opioid and alcohol use disorders.
Family participation and support
Recovery doesn’t happen in isolation. Many IOPs invite family members or other loved one supports to participate in treatment through structured education and therapy sessions.
What family involvement looks like:
- Family education nights covering topics like understanding addiction or mental illness as a chronic condition
- Multi-family groups where several families learn and share together
- Structured family therapy addressing communication patterns, boundary-setting, and healing relationship damage
- Guidance on recognizing warning signs of relapse or symptom worsening
Topics typically include how to set healthy boundaries, communicate without escalating conflict, and support recovery without enabling harmful behaviors.
Participation is always voluntary and guided by your consent and privacy laws like HIPAA. You decide who’s involved and to what extent. Research consistently shows that family involvement improves treatment adherence, reduces relapse risk, and increases satisfaction—for both the person in treatment and their family members.
Evidence-Based Approaches Used in Intensive Outpatient Programs
Modern IOPs rely on therapies tested through rigorous research and endorsed by organizations like NIDA, NIAAA, and SAMHSA. These aren’t experimental approaches—they’re proven methods with decades of evidence behind them.
Different evidence-based approaches are used to treat various substance use disorders and mental health conditions. No single method works for every person. That’s why most programs blend multiple approaches—combining cognitive behavioral therapy with motivational interviewing, or integrating 12-Step facilitation with skills training. Your treatment plan will reflect what works best for your situation.
Cognitive-Behavioral Therapy (CBT)
Cognitive behavioral therapy is a structured approach that helps you identify and change the thought patterns and behaviors fueling depression, anxiety, or substance use. It’s one of the most researched therapies in behavioral healthcare, with decades of evidence showing effectiveness for both mental health conditions and substance use disorders.
Core CBT skills you’ll practice in IOP:
- Identifying high-risk situations and automatic negative thoughts
- Challenging distorted thinking with evidence and alternative perspectives
- Building concrete coping plans for specific triggers
- Problem-solving step-by-step when challenges arise
- Tracking moods, thoughts, and behaviors between sessions
IOP is particularly well-suited for CBT because you practice strategies in daily life after each group, then report back the next session. This real-world testing accelerates learning and helps you manage symptoms more effectively than practicing in a controlled environment alone.
Motivational Interviewing and Motivational Enhancement (MI/MET)
Motivational interviewing is a conversational approach that respects your ambivalence about change. Rather than pushing you toward a goal you’re not ready for, MI uses empathy and open-ended questions to strengthen your own internal motivation.
How MI works in IOP:
- Clinicians explore the pros and cons of current patterns without judgment
- You articulate your own reasons for change, which strengthens commitment
- Sessions help you move from “I should change” to “I want to change”
- MET adds structured assessments and personalized feedback showing patterns in your use, mood, or consequences
Examples of MI-style questions you might hear:
- “What concerns you most about your current situation?”
- “On a scale of 1–10, how important is it for you to make a change?”
- “What would your life look like if things were different?”
International studies show MI produces meaningful reductions in drinking and drug use, even in brief formats. It’s especially helpful early in treatment when motivation is still developing.
12-Step facilitation and mutual-help integration
12-Step facilitation is a professional therapy approach that introduces you to recovery fellowships like Alcoholics Anonymous, Narcotics Anonymous, and other peer support communities. A key goal of 12-Step facilitation is to help clients achieve abstinence through active participation in these groups.
What this looks like in practice:
- Learning the 12 Steps and their underlying principles
- Addressing common misconceptions about what meetings involve
- Help finding local meetings that match your schedule and preferences
- Encouragement to connect with a sponsor who can guide your recovery
Community meetings happen outside IOP hours and complement—rather than replace—professional therapy. For people with more severe substance use patterns, research shows 12-Step–oriented approaches are particularly helpful for building long-term recovery support. In fact, studies indicate that the 12-Step facilitation approach provided more favorable outcomes for most people who abuse substances compared to structured relapse prevention.
Not everyone connects with 12-Step programs, and that’s okay. Many IOPs also introduce alternatives like SMART Recovery or Refuge Recovery for those who prefer different frameworks.
Matrix Model and structured addiction protocols
The Matrix Model is a highly structured intensive outpatient treatment approach originally developed in the 1980s for people with stimulant addictions like cocaine and methamphetamine. The Matrix Model is specifically designed to treat stimulant dependence and other substance use disorders, and its principles are adapted for broader use across addiction treatment programs. In a 1985 pilot study, individuals who selected Matrix treatment over a 28-day inpatient hospital program reported significantly lower rates of cocaine use 8 months after treatment than those in either of the other groups.
Therapeutic communities (TCs) use a community-based approach to treatment, focusing on mutual help and social learning. Clients who completed TC treatment had lower levels of cocaine, heroin, and alcohol use; criminal behavior; unemployment; and depression than they had before treatment.
Community reinforcement and contingency management (CR/CM) approaches motivate clients’ behavioral change and reinforce abstinence by systematically rewarding desirable behaviors. Studies show that the CM approach to treating substance use disorders has proved effective in motivating clients to achieve and sustain abstinence as well as increase their compliance with other treatment objectives.
Key elements of Matrix-style treatment:
- CBT-based relapse prevention strategies delivered in structured group and individual sessions
- Motivational techniques woven throughout to build and maintain engagement
- Regular family education sessions addressing the entire household’s role in recovery
- Routine urine testing to support accountability and identify slip-ups early
- Strong emphasis on the therapeutic relationship between clinician and patient
The original 16-week Matrix protocol includes structured phases with specific objectives—participants progress based on meeting goals, not simply passing time. Long-term studies show substantial decreases in stimulant use for people who complete Matrix-based care.
Many modern IOPs incorporate Matrix-style tools like weekly worksheets, progress checklists, and phase systems, even if they’re not branded as official Matrix programs.
Length of Stay and Typical IOP Schedule
Most intensive outpatient programs last 6–12 weeks, though length varies based on your progress, clinical need, and insurance approval. Some substance use programs extend to 90 days or longer, especially when combined with sober living arrangements.
Weekly time commitments typically fall into these ranges:
- Minimum: 9 hours per week (often 3 days × 3 hours)
- Standard: 9–15 hours per week for most mental health and substance use IOPs
- Higher intensity: Up to 19 hours weekly for those needing more structure
A sample weekly schedule might look like this:
You attend group sessions on Monday, Tuesday, and Thursday evenings from 6:00 p.m. to 9:00 p.m.—a total of 9 hours. Every other Wednesday, you have a 50-minute individual therapy session with your primary counselor. Twice monthly, your spouse or a family member joins for a family education group on Thursday before regular programming. As you progress, your team may reduce attendance to two days weekly while adding a weekly aftercare group to prepare for transition.
This flexibility means your schedule evolves with your needs rather than forcing you into a rigid structure that doesn’t account for real-life demands.
Is an Intensive Outpatient Program Right for You?
Choosing the right level of care starts with honest reflection about your current situation. Consider your safety, your support system, your substance use patterns, and your ability to manage daily responsibilities while attending sessions.
Signs that IOP may be a good fit:
- You have stable housing and a relatively safe environment to return to each day
- You don’t currently need medical detox or supervision for withdrawal symptoms
- Your symptoms are significant but manageable between sessions with appropriate support
- You’re motivated to attend treatment multiple times per week
- You have some social support—or you’re willing to build it through the program
- You can manage routine activities like work, school, or childcare with scheduling adjustments
Signs you may need a higher level of care:
- Recent suicide attempt or active suicidal planning with intent
- Uncontrolled psychosis, severe mania, or inability to care for yourself
- Severe medical complications like uncontrolled seizures or high risk of delirium tremens
- History of serious withdrawal complications that require medical supervision
- Inability to remain safe between sessions due to environment or impulse control
The decision should be collaborative. Talk with a physician, psychiatrist, or licensed therapist who can complete a thorough assessment and help you choose between inpatient, PHP, and IOP. Many people move stepwise through levels of care—inpatient to PHP to IOP to standard outpatient to support groups—rather than viewing any single level as a complete solution.
Recovery is a process, and the right level of care today may shift as you progress.
Finding an Intensive Outpatient Program Near You
Outpatient programs are widely available through hospitals, community mental health centers, nonprofit agencies, and private treatment networks across the United States. Finding the right fit takes a little research, but help is more accessible than many people realize.
Practical strategies for your search:
- Search your insurance company’s provider directory for “intensive outpatient” or “IOP”
- Use search terms like “intensive outpatient program near me” along with your city and state
- Check SAMHSA’s national treatment locator at findtreatment.gov
- Contact local hospitals and ask about behavioral health or addiction treatment outpatient programs
- Ask your primary care physician or therapist for referrals
Questions to ask when you call a program:
- How many hours per week does the program provide?
- What are staff credentials and specializations?
- Are there age-specific or condition-specific tracks?
- Is telehealth available if I can’t attend in person?
- What’s the current waitlist time?
- How does the program handle aftercare planning?
- Call your insurance company’s behavioral health line before starting
- Ask about copays, deductibles, and any session limits
- Clarify whether medications, labs, or psychiatric visits are billed separately
- Request pre-authorization if required by your plan
Consider requesting a brief phone or virtual intake before committing. This gives you a chance to see if you feel comfortable with the team and format—an important factor in whether treatment works.
How to Get Started with IOP
Beginning your journey toward healing through an intensive outpatient program starts with a few meaningful steps that honor where you are right now and where you want to go. The first step is reaching out to a primary care physician, mental health provider, or addiction treatment specialist—and taking that step shows incredible courage. These compassionate professionals will sit with you through a thorough assessment of your mental health, substance use, and your unique story to determine if IOP treatment is the right path for your recovery.
Once IOP is recommended for your journey, the next step is finding a facility that truly understands you and your needs. As you research your options, consider what matters most: the program’s heart and reputation, the range of healing services they provide, the expertise and warmth of their clinical team, and whether they work with your insurance to remove barriers to care. Many programs offer flexible scheduling—morning, afternoon, or evening sessions—because they understand that recovery must fit into your real life. For those who need additional flexibility, some facilities provide online intensive outpatient services, allowing you to attend treatment sessions from the comfort and safety of your own home.
Taking these steps ensures that you can access high-quality, client-centered care that’s tailored specifically to your unique circumstances and your story. With the right support and a structured treatment plan that honors your journey, you can begin the process of transformation and work toward lasting wellness that goes far beyond just surviving—this is about thriving, healing that lasts, and creating your new beginning.
Taking the first step toward IOP treatment is exactly that—a step, not a commitment you can’t adjust. If you’re wondering whether this level of care fits your situation, reaching out for an assessment is the clearest path to an answer. Help is closer than you might think, and recovery starts whenever you’re ready.
Whether you’re supporting yourself or a loved one, you don’t have to figure this out alone. Let’s walk through the next steps together.
Frequently Asked
Questions about Intensive Outpatient Programs
What is an IOP and why is it used?
An Intensive Outpatient Program (IOP) is a treatment program designed to help individuals recover from:
-
Substance use disorders (SUD)
-
Mental health conditions
-
Dual diagnosis (co-occurring disorders)
IOPs are used when:
-
Inpatient or residential care is not clinically required
-
A higher level of support than weekly therapy is needed
-
Patients need structure while maintaining work, school, or family responsibilities
IOPs are widely recommended by SAMHSA, ASAM, and major healthcare systems as an effective step-down or alternative to inpatient care.
How many hours is an intensive outpatient?
Most IOPs provide:
-
9 to 20 hours of treatment per week
-
Typically 3–5 days per week
-
Sessions lasting 3–4 hours per day
Exact hours vary based on:
-
Clinical needs
-
State regulations
-
Insurance requirements
Who qualifies for an intensive outpatient program?
You may qualify for IOP if you:
-
Have mild to moderate substance use disorder
-
Are medically stable and do not require detox
-
Need structured treatment but can live independently
-
Are stepping down from inpatient or residential care
Clinical determination is usually made using ASAM criteria and a professional assessment.
What happens after I complete IOP?
After completing IOP, patients typically transition to:
-
Standard outpatient therapy
-
Aftercare or relapse prevention programs
-
Peer support groups (AA, SMART Recovery, etc.)
-
Continued psychiatric or medication management
According to SAMHSA, continuity of care significantly improves long-term recovery outcomes.
Can I work or go to school while attending IOP?
Yes. IOPs are specifically designed to allow patients to:
-
Maintain employment
-
Attend school
-
Care for family members
Programs often offer:
-
Evening schedules
-
Flexible session blocks
-
Virtual attendance options
How do virtual IOPs compare to in-person programs?
Virtual IOPs (telehealth-based programs) provide:
-
The same clinical structure
-
Licensed therapists and group sessions
-
HIPAA-compliant platforms
Research cited by SAMHSA indicates virtual IOPs can be equally effective for many patients, especially those with:
-
Transportation barriers
-
Work or childcare constraints
-
Social anxiety or mobility limitations
How much does an intensive outpatient program cost, and will insurance cover it?
IOP costs vary by provider, location, and services offered, but typically range from:
-
$3,000 to $10,000 per week without insurance
Most private insurance plans, Medicaid, and Medicare cover IOP when:
-
Medical necessity criteria are met
-
Preauthorization is completed
Coverage standards follow Affordable Care Act (ACA) behavioral health parity requirements.













